It is mid-summer 2017 and Pablo Lievano is fishing. It is early in the day – the best time to fish, and also to plan for the busy day ahead. Waist-deep in the cool water he delicately casts his favourite hand-tied fly ‘Pablo’s Demon’ into the current.
This moment of calm was shattered by a seizure. Luckily Pablo made it safely to the riverbank and to help. The devastating diagnosis of Glioblastoma rapidly followed with Pablo hearing the words “you have a brain tumour” in September 2017. It is this tumultuous opening where our story starts predicating an incredible collaboration and friendship.
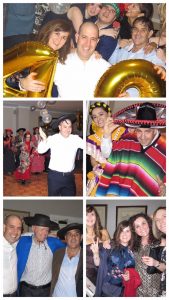
Pablo was determined not to let his diagnosis impact negatively on the time he had ahead of him. He set out to live life to the full, surrounded by family and friends, and seeking solace in fly-fishing. Following early fears, Pablo’s resilience was buoyed by his diagnosis and he developed an incredible determination to become the ‘captain of his cancer’. Resolutely he focussed on his own and his family’s wellbeing. He tackled the challenges that he could proactively, passionately and with vigour. But he did not stop here. He set out to inspire as many others on the same journey to do the same.
Pablo contacted brainstrust early on his journey as he explored holistic support beyond the discussion of treatments and trials that fill hospital clinics. Unusually though he contacted brainstrust less to seek help, and more to establish how he could help others.
Pablo took his story and his mission to his workplace, to the Prime Minister, to the Queen, and even to the Pope whose blessing he received. He worked selflessly to raise awareness of the importance of wellbeing when you are living with brain cancer. And in parallel, with his ‘A-team’, he helped hundreds of others who were walking in the same shoes. He painted an inspiring and sometimes formidable picture that showed that nearly anything is possible when you put your heart and soul behind it. Through his tenacity Pablo worked with his doctors to access hard-to-get and early stage treatments. These included Tumour Treating Fields (TTF), radiosurgery and Cannabinoids. True to form he tried them and reported on the effects honestly so that others could learn from his own experiences. He threw everything he could at overcoming his brain tumour so that he could enjoy a longer life with his family, but with always a weather eye on the impact that these treatments were having on his wellbeing.
It was Pablo’s passion and our shared belief that ‘first we are people, second we are patients’ that led us to work collaboratively on the Wellbeing events at Cliveden House. These have helped well over 100 people directly and are one of the highest scoring events on the brainstrust calendar in terms of direct impact for participants. Only Pablo’s tenacity and good humour could have unlocked the doors of such a special venue and made it accessible for our community, but he did not stop until Cliveden pledged to nominate brainstrust as its charity of the year.
With family, friends and colleagues, Pablo fundraised tirelessly and with single-minded focus on his aims. He secured over £8000 for wellbeing projects that will directly benefit people with a brain tumour.
Pablo was one of us. He was a true member of our community, but he was also one of our community’s greatest advocates. He was unafraid to challenge the status quo: anything but a holistic approach to brain tumour care was unacceptable. And it is in this outlook that his legacy will become a rich part of brainstrust’s story for years to come.
From the point of his diagnosis Pablo told us repeatedly that he had newfound purpose and vigour, and that he had found his true calling in helping others. His diagnosis brought him new meaning. But the brightest of stars only burn for the shortest of times, and last week Pablo passed away. He died of his brain tumour during the night on Wednesday 31st July, and is survived by his wife Maria, and young son, Sebastian.
You can find out more about the events that Pablo helped to make happen here.
Read a write up of the most recent event here.
If you’d like to donate to fund more of these events in Pablo’s memories, please click here.