Counselling support for brain tumour patients and their caregivers
Counselling creates the space for you to talk through your feelings in a safe and confidential place. It will help you to develop strategies for managing your future. It comes into play when support is needed to understand psychological distress associated with, what is sometimes referred to as, “problems with living”.
For example, it may be helpful for someone who is struggling to cope or feeling very anxious or depressed. Counselling tends to have a broader focus and greater depth than coaching. It helps people to explore and understand the feelings which are causing them grief and to identify and explore steps for moving beyond these feelings to make positive changes in their lives. Counselling can be very challenging as it can often unearth very painful feelings, make people confront unresolved personal issues and challenge them to change the way they go about their lives today and in the future. Counsellors help people by building a supportive relationship which is based on the essential qualities of acceptance/warmth, genuineness and empathy. Like coaching, they do not offer solutions or advice, but instead help the client to identify their own issues and ways of moving forward.

You can download more information about counselling for people affected by brain tumour here.
If you would like to find out more about this service then you can call our helpline on 01983 292 405, or email hello@brainstrust.org.uk
We are able to provide fast track access to counselling for people with a brain tumour, and their caregivers thanks to the generous support of Lloyd’s Legacy, and the Souter Charitable Trust.
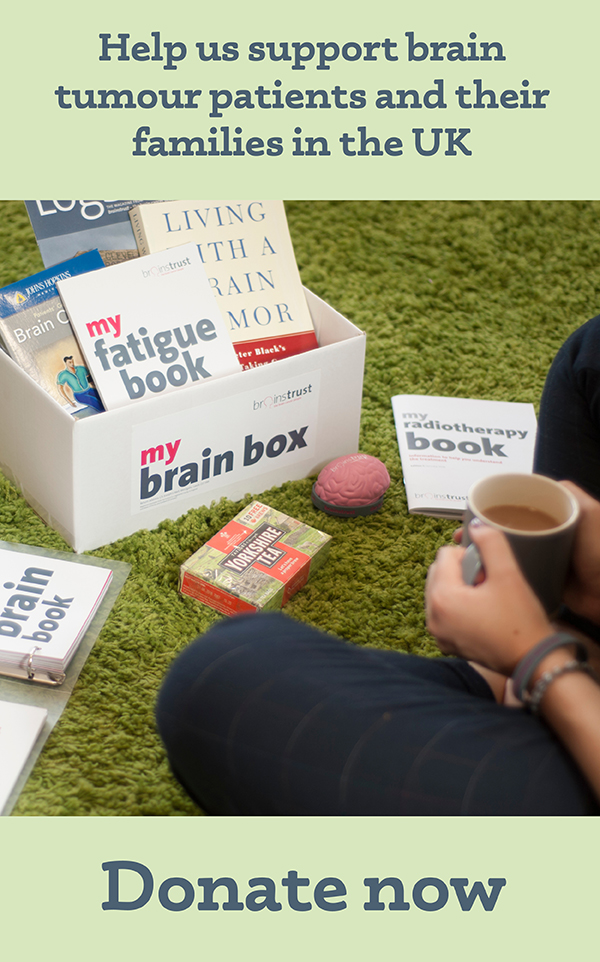
Discover our resources, designed to help you feel less alone and more in control.
Hypnotherapy for brain tumour patients and their caregivers
When you are living with a brain tumour, or are caring for someone living with a brain tumour, you may find hypnotherapy useful in improving wellbeing in the following areas:
- Anxiety and stress
- Diet and lifestyle
- Resilience, self esteem and confidence
- Pre and post-operative care
- Pain management
- Reduction of side effects from treatment such as nausea, fatigue
We’re delighted to have Louise Baker (MSc Psychology and Neuroscience of Mental Health) working with brainstrust as our own consultant hypnotherapist.
Louise is an experienced trainer of Hypnotherapy, NLP Master Practitioner, coach and Time Line therapist. She holds diplomas in Clinical Hypnotherapy, Hypnotherapy and Psychotherapy and has a Specialist Certificate in Past-Life Regression.
Louise Baker has many years experience as a Clinical Hypnotherapist, having helped hundreds of clients deal with a wide range of issues. She is passionate about hypnotherapy and is really pleased be able to support people affected by a brain tumour.
‘I love helping people change and achieve a sense of well being. By working with me, you can clearly identify what you want and take the steps needed to get there.’

Interested in hypnotherapy or need more information?
Just call brainstrust to discuss your situation in complete confidence 01983 292405 or email hello@brainstrust.org.uk.
Calmness and Connectivity online sessions
Recently retired from 1:1 work, Louise is now focused on bringing the power of this work to groups for brainstrust through our Calmness and Connectivity webinar series.
We are pleased to be able to run two sessions a month, each of them hosted by Louise alongside a brainstrust Support Specialist. We run an afternoon and an evening session- each of which are made up of two parts, to help you gain a deeper understanding of hypnotherapy and practice the techniques discussed in a safe and welcoming environment.