Feel less alone as a caregiver
We know that being a caregiver for someone with a brain tumour can be lonely and isolating. On this page you will find information to help you feel less alone and better supported.
Becoming a Caregiver
We know when faced with a brain tumour diagnosis that it not only affects the person with the diagnosis, but also those close to them.
A Caregiver is someone who provides unpaid help and support to a family member, friend or neighbour who would otherwise not be able to manage without this support.
Many people that provide help and support to those close to them who are affected by a brain tumour diagnosis, don’t classify themselves as a caregiver.
Caring for someone with a brain tumour can sometimes be more challenging due to the complexity of the pathway, and at times the uncertainty that can come at different stages along this.
Becoming a caregiver for someone with a brain tumour can happen abruptly or creep in slowly unnoticed until one day you realise you are caring more for someone else than you are for yourself.
Support for you
When you suddenly find yourself taking on the role of a Caregiver due to a loved one’s brain tumour diagnosis, priorities shift and sometimes your own needs take a backseat.
The role of a Caregiver can at times be complex, stressful and also isolating due to the tasks you may find yourself suddenly having to take on. These could include having to help with personal care, giving physical nursing care without any additional support, providing transport as well as providing emotional support to your loved one and trying to source information and support.
In order to care, you need to take care of yourself. Seeking out help before you really need it may help you to feel more in control and resilient just by knowing that there are options.
There are many organisations who can offer support for Caregivers. Support can come in a variety of different ways- whether that be physical support or emotional support.
For details of the organisations that may be able to help, visit our brain tumour hub: https://www.brainstrust.org.uk/brain-tumour-hub/
Coaching to help you thrive
At brainstrust we have a team of trained coaches. We listen, listen some more and then ask questions.
We focus on helping you achieve specific immediate goals, which relate to specific areas. For example, weighing up the pros and cons of having a particular treatment, or overcoming a problem with caring. We also know that through coaching, clients can experience a sense of healing, as they make decisions about their lives.
Coaching is about developing strategies and clarity to achieve a better quality of life.
If you would like to know more about coaching or to arrange a conversation with one of our coaches, get in touch with us at hello@brainstrust.org.uk or call our helpline on 01983 292 405
Counselling
When there is too much distress and a psychological intervention is needed, counselling can be useful.
It is suitable for someone who is struggling to cope or feeling very anxious and therefore finding it hard to focus on specific immediate goals. We have a network of counsellors who can help you make sense of your situation, so that you can make better decisions about the future.
For more information about counselling, just visit this page: https://brainstrust.org.uk/brain-tumour-support/quality-of-life/living-well-with-a-brain-tumour/counsellinghypnotherapy/
First steps – What to do when you hear the diagnosis
The possibility that the person for whom you are caring might have a brain tumour will have been on your mind, but you never know how you will react until you actually hear the news.
You will be reeling but your ability to cope does get better – you develop systems to cope with such traumatic change. And it is so hard being the person that loves the afflicted so much that it hurts; you just want to give the person hope and try to hold it together for all around. those around you and how they will cope. You want to reassure yet you yourself are feeling very frightened.
What you want to know is that you have explored every avenue and have done everything that you can be doing to help; it is at this stage where your role as a caregiver may take on more of a ‘management role’.
Here are some tips of how you can feel prepared at this stage of the pathway:
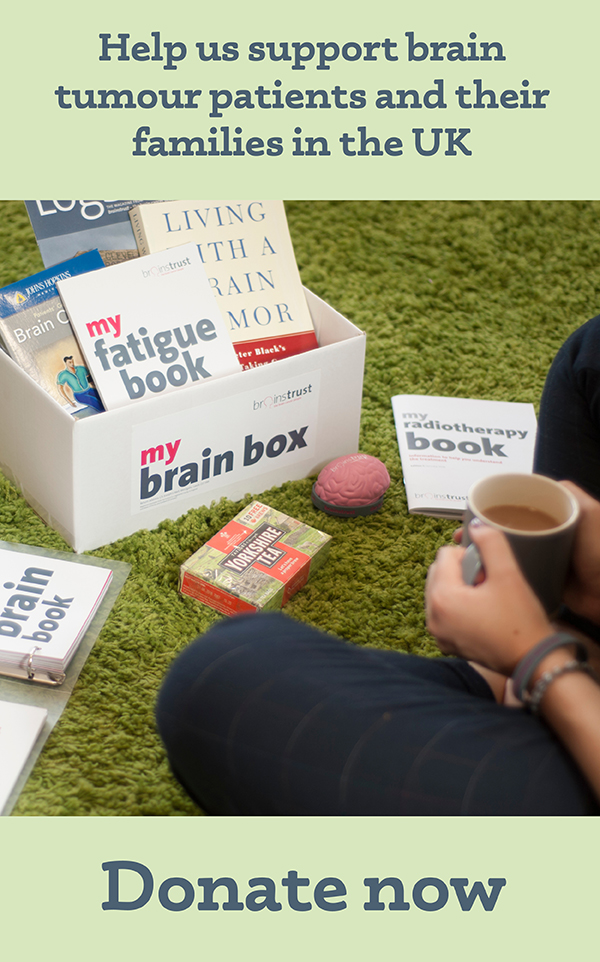
- Get a notebook which you can take to all appointments and take key notes- ‘My brain book’ which is included in the brain box is a brilliant way to keep all these notes organised.
- Ask questions- refer to the ‘Diagnosis’ patient guide, which can be found here: brainstrust.org.uk/brain-tumour-support/resources/downloads/ This has some good questions to get you started, as well as information about what you should expect at this stage.
- Find out who is in your team. By ‘team’ we mean both the clinical team, but also who can help you outside of the hospital. This can be friends or family members or charities. It is important to build a supportive team around you. This Know How will help.
- Call us on the 24/7 helpline. We’ll be here to make sure you are confident that you are getting the best care and help you with questions (no matter how big or small) that you have- we don’t always have the answers, but we can help you work out what you need to do to get what you need.
- Don’t forget the ‘you’ in all of this: you too need to look after yourself. You can read more about how to do this here.
Discover our resources, designed to help you feel less alone and more in control.