Exercise and rest
There is evidence to show that exercise can help your body to work at its best when you are living with a brain tumour[1]. Exercise can improve strength, fitness, mood and general wellbeing. But exercise isn’t always straightforward when you have a brain tumour.
Exercise
The brain controls voluntary movement, balance and gait, all essential elements of physical activity. When the brain’s occipital lobe is affected, some vision can be lost as well, making mobility more difficult. In addition, therapies can cause fatigue, dizziness, weakness and lack of balance, making the situation worse. And long-term use of steroids, which may be given to counteract chemotherapy side-effects, also cause muscle wasting.
So exercise may be particularly difficult for some people living with a brain tumour. Equally though, exercise may bring the greatest benefit. The most important thing is to do what works for you. For many, walking is easy to build into daily activity. Others choose yoga, workouts in the gym, cycling, swimming or sports.
If balance is a problem, exercises can be done whilst sitting down. You could practice standing while lightly holding on to a kitchen worktop or heavy piece of furniture. Let go of it intermittently, but stay close enough so you can grab onto it again if you need it.
Exercise in short sessions for three to five minutes a few times a day, rather than longer single sessions.
Add gentle stretching exercises to your regimen. Yoga is great for building strength and for relaxation.
Don’t underestimate the benefits of going for a walk. The payback is huge, but pace yourself. If you haven’t been for a walk for a while, set a realistic goal of five minutes, gradually increasing the time until you are walking for thirty minutes. Walking will help you to:
- maintain a healthy weight
- increase your energy levels
- prevent or manage various conditions, including heart disease, high blood pressure and type 2 diabetes
- strengthen your bones and muscles
- improve your mood
- improve your balance and coordination
[1] Ruden, E. et al. (2011). Exercise behavior, functional capacity, and survival in adults with malignant recurrent glioma. Journal of Clinical Oncology, 29(21), pp. 2918–2923
Rest
The antithesis of exercise. What does rest look like for you? It means different things for different people and is never a case of one size fits all. Rest is important. It stops you getting to the point of exhaustion so that you have to stop what you are doing, regardless of what you are doing. Planning for rest is a critical part of managing your condition. By planning your activities, you can plan to rest too. Only you know what type of rest break works for you, for how long and when. It could be:
- a few short rests, or power naps
- one longer rest at the same time each day
- resting between activities.
Try not to nap after 3 p.m. and only nap for up to twenty minutes. The quality of rest is key. Try to make your rest as complete as possible. This means aiming to switch of your mind and body and, more importantly, asking those around you to understand how valuable this time is for you. You need to be quiet and undisturbed.
Online fitness for people with a brain tumour
 CUFitterXtra is a 12 week online programme for people affected by cancer or a brain tumour. Operated by Cancer United, CUFitterXtra matches you with specialist trainers who are experienced working with people living with a cancer diagnosis and/or preparing, undergoing or recovering from oncology treatment.
CUFitterXtra is a 12 week online programme for people affected by cancer or a brain tumour. Operated by Cancer United, CUFitterXtra matches you with specialist trainers who are experienced working with people living with a cancer diagnosis and/or preparing, undergoing or recovering from oncology treatment.
brainstrust has teamed up with the Cancer United team to bring this programme to people living with a brain tumour diagnosis.
What does the programme involve?
At a total price of £60, you get access to the following:
- Initial 12 week online video fitness programme
- Tailored classes to suit you
- Initial online consultation to place you in the right programme
- 1 new video sent by email every week for 12 weeks
- Mid-programme assessment online consultation
- Online helpdesk to answer any questions or issues
The programme offers flexibility so that you can adapt the programme in a way that works best for you and your diagnosis:
- Exercise from the safety of your own home
- Access your weekly video at a time that works for you
- Exercise with the video as many times as you want
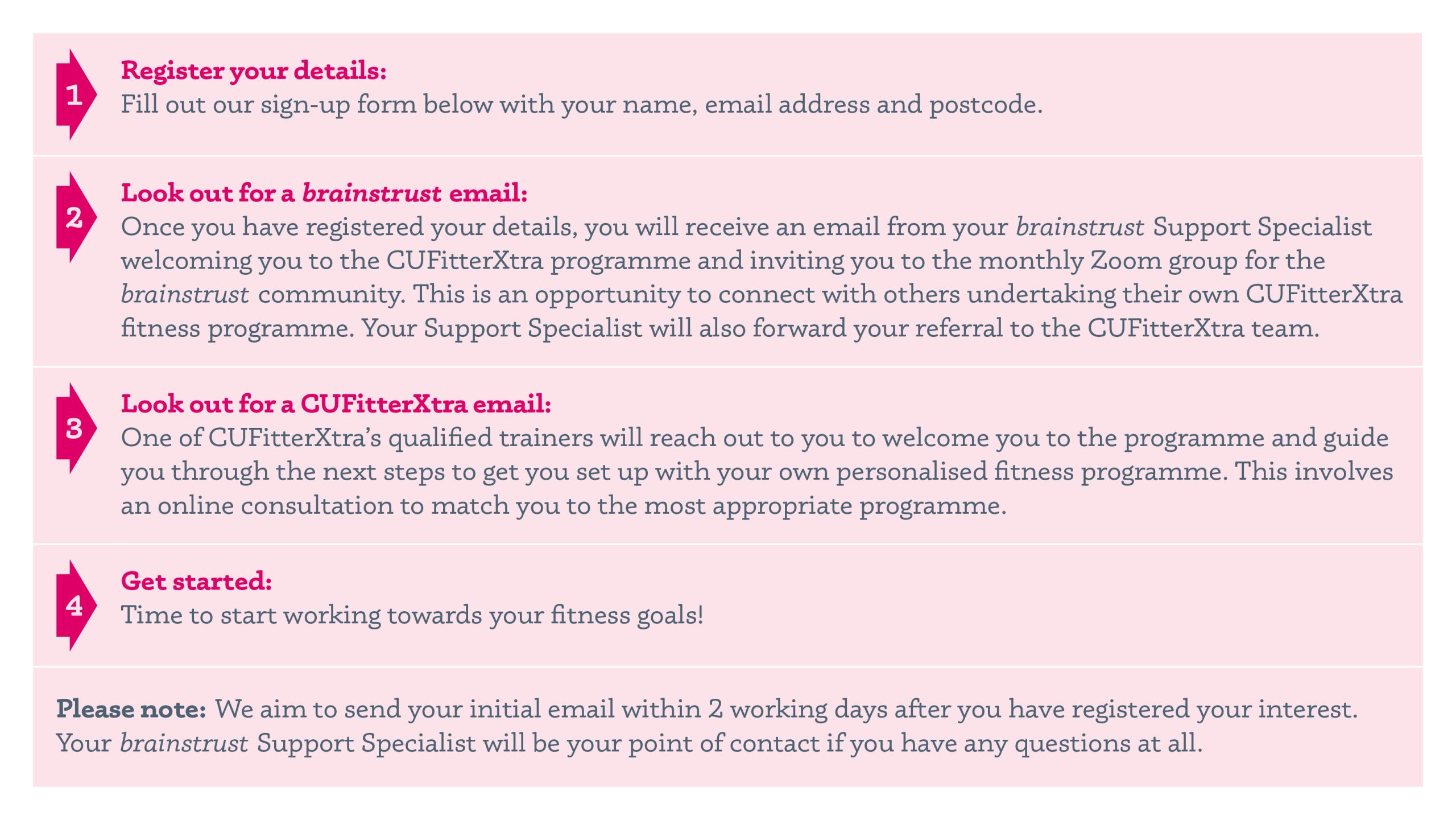
Fill out the form below to register your interest
To register your interest, enter your details below and a member of the brainstrust support team will get in touch to guide you through the next steps of signing up for the CUFitterXtra programme.
We will also invite you to join our regular online CUFitterXtra buddies group, should you wish to connect with others completing their own programme and perhaps find an accountability buddy. We are here to cheer you on every step of the way!
Please note, the CUFitterXtra service is only available to patients that have or have had a brain tumour, it’s not available to caregivers or loved ones.