The British Neuro-oncology Society conference, Liverpool 2022- current, innovative and alternative; raising the standard.
The human being is the most technologically equipped thing in the operating room –
Ryan Matthew, Associate Professor at the University of Leeds and Honorary Consultant Neurosurgeon at the Leeds Teaching Hospitals NHS Trust, BNOS 2022.
Ryan’s wise and eloquent words sum up the BNOS conference 2022. This was the first face-to-face BNOS since 2019 and it is evident that, despite the COVID-19 tidal wave, people have been incubating ideas, working on projects and using any space to reflect, take stock and explore. And central to everything we heard in Liverpool is the person living with the brain tumour. We can’t possibly cover everything here, but over the next few weeks we will be sharing recordings, soundbites, research and our commentary about what is relevant and meaningful for the community. What we may not be able to do is capture the energy and buzz from the conference.
Marginal gains
There is a sense that things are shifting, the new knowledge we have about genomics and technological developments facilitates the view of the whole patient pathway as one seamless thread. This feels very much live David Brailsford’s principle of marginal gains. This principle was transformative for the British cycling team; it had been struggling to perform, limited by their “big picture” view of winning, they had failed to reach the Olympic podium for decades. Brailsford took the notion that small, incremental improvements across a range of things, when added together, can make a significant improvement. This sense pervaded the conference.
1. Dave Bolton
So let’s look at four highlights. The first has to be the inspirational talk by Dave Bolton, who led on mental resilience and coping with change. Dave’s first battle was being run over by an articulated lorry when he came off his motorbike on the Horseshoe Pass in Wales. He’d just got back on his feet (literally) and was flying in his career when he diagnosed with a grade 2 astrocytoma in 2014. This transformed to a high grade in 2015 and he had a full psychotic breakdown due to medication. Today? He is super fit, runs everywhere, and leads a highly regarded cancer prehab and rehab centre.
2. Patient pathways
This is a great segue to the next highlight about the patient pathway. There was a sense of awareness of the whole pathway, with sessions on cognitive evaluation and rehabilitation, integrated enhanced recovery led through multidisciplinary teams, a review of health-related quality of life research, the role of prehabilitation and core outcome sets. As ever, the patient and their caregiver is the mortar here, and it is down to our community that we are able to represent its voice. This isn’t just about diagnosis, or recurrence, or living with; this is about managing transitions so that patients and their caregivers are confident about navigating their path, which is individual to them. We are looking at how all of these things, whilst complex, can work together to be a seamless experience.
3. What’s new in neuro-oncology neurosurgery
Neurosurgical approaches too have their names up in lights. Ryan Mathew, Associate Professor and Honorary Consultant Neurosurgeon at the University of Leeds gave a forward-looking presentation on what’s new in neuro-oncology neurosurgery. The goals of neurosurgery are twofold – to preserve function, whilst maximising the amount of tumour tissue that can be removed. This is the bottom line. But Ryan showed us all how things are shifting, pre-operatively, during surgery and also post-operatively. Exploring how residual tissue at the margins of the tumour can be removed is one area, another is the local delivery of therapies to the tumour site during surgery, and a third is the paucity of data that we currently have around surgery – ‘the information wedge’. Closing the gap between the lab and the operating room, so that the lab is an extension of the operating room will bring imaging, molecular analysis, histopathology in a synchronous whole.
4. Genomics
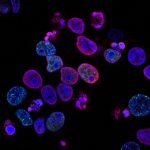
Finally – genomics. Such a massive topic. Biomarkers are key for the development of individualised and targeted therapy. The fact that the World Health Organisation has had to update the categorisation of brain tumours twice (2016, 2021) illustrates how far we have travelled. More and more we are now discovering subsets of tumours, all of which have their own footprint, all of which will drive biomarker-decision making. But there is still a disconnect between what we now know and what treatments are available. We can’t though achieve one without the other, and whilst it is good news that we know so much more about the make up of tumours, it does of course mean that the approach is increasingly granular so we will have even smaller subsets of patients in which to test therapies.
So – just a taste of BNOS 2022. We will share highlights in much more detail in the next few weeks. After all, the people living with the brain tumour are the only source of data – and it was heartening to see how much the patient experience was in the DNA of this conference. We’d like to thank the organising committee, led by Andrew Brodbelt and all of the presenters, for bringing so much to the community.