Navigating your pathway
It can be daunting navigating your brain tumour pathway, but we can help you on your brain tumour journey no matter where you are in the process. Whether you want information about brain tumours and treatment, or access to resources that will help you feel more in control, we’re here every step of the way.
Use the links below to access the information you need, and don’t forget there are various ways you can reach out to us for support. Send us a message on our website chatbot, call us on 01983 292405 or email us at hello@brainstrust.org.uk. We’re here for you whenever you need us.
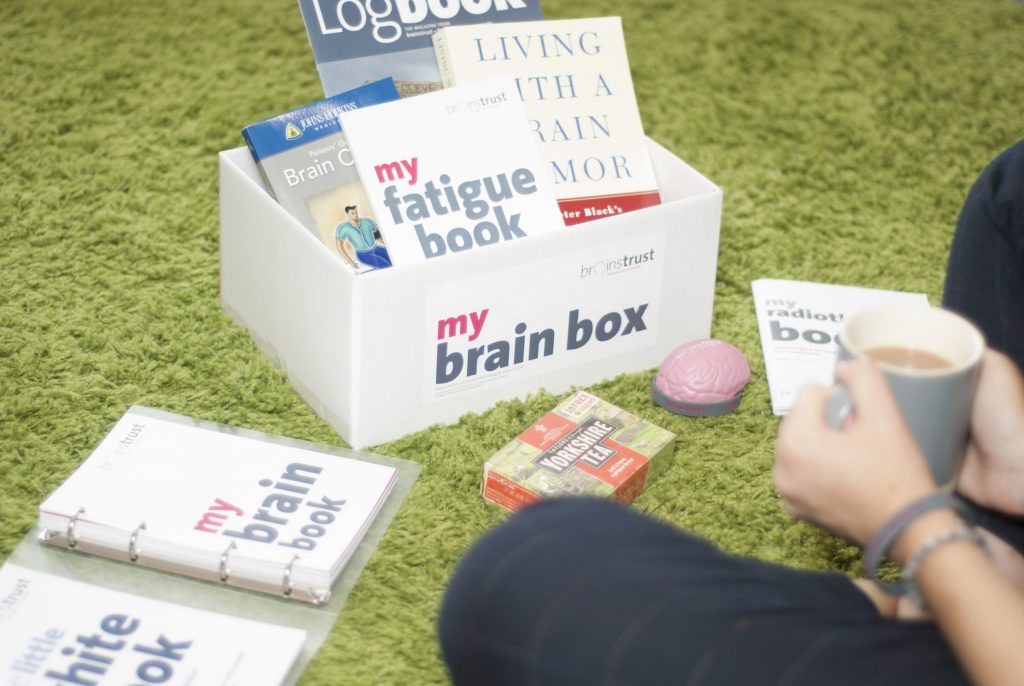
Our patient guides cover every stage of the brain tumour pathway.
For information and support for a meningioma diagnosis visit our dedicated site.