Navigating your pathway
Living with a brain tumour is bewildering, isolating and scary. There are key things you should be doing that will help. One is to keep records of everything (our patient folder which comes with our brain box helps here) and the other is to always get a copy set of your MRI scans. As a patient, this is your data – it belongs to you. Ask your imaging department for a copy set.
Having the information that you need at your fingertips can transform the feeling of control that you have, whether you are a patient or a caregiver.
On this page you will find:
- What to expect from your pathway
- The Neuroscience Multidisciplinary Team (MDT)
A typical pathway
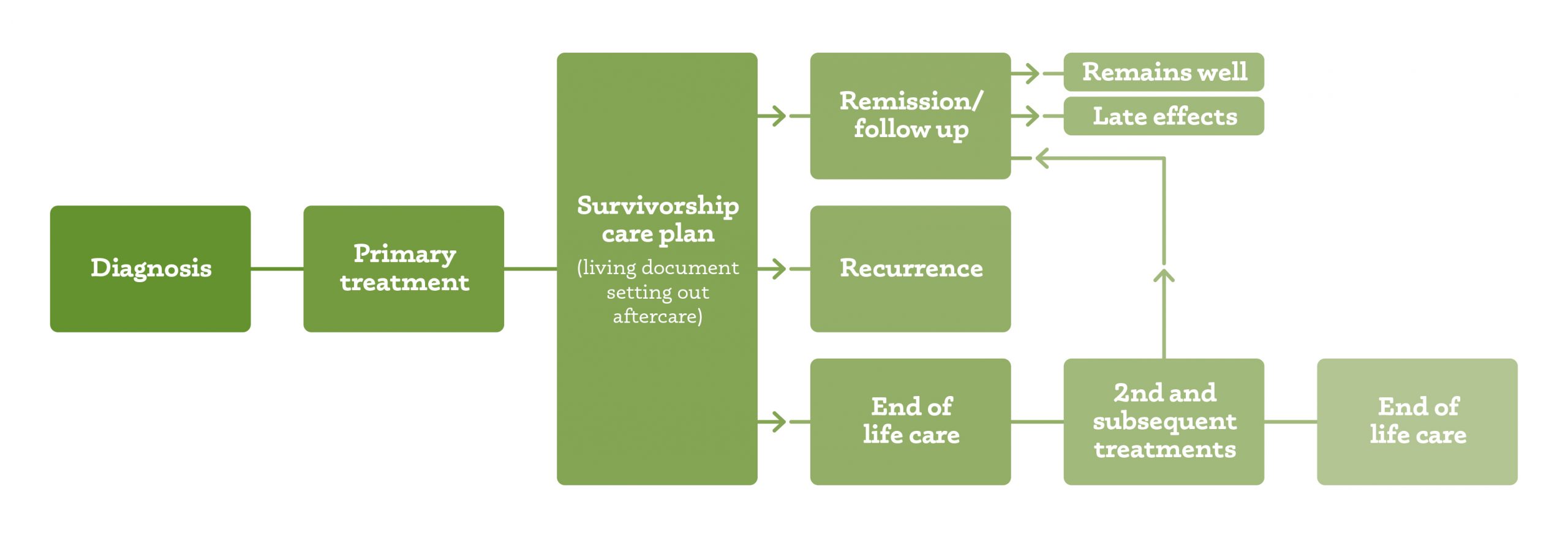
But nobody is ‘typical’ – and when you add in the fact that there are many different types of brain tumours, all of which have different prognoses and their own idiosyncrasies, this kind of pathway is only ever going to be big picture.
So use our patient guides to help you navigate. This is the only comprehensive, easy to understand guide of the adult brain tumour pathway. They will help you to know more about what to expect so that you can feel more in control.
And of course, for those particularly thorny questions you can always email hello@brainstrust.org.uk or call 01983 292405.
The Neuroscience Multidisciplinary Team (MDT)
We’re great believers in knowing the big picture, then you know what your options are. Equally, though, we know that not everyone wants to know about their diagnosis. Everybody has a different way of dealing with an illness. So this information is for you to use – or not. It’s up to you. And of course, even if you have made a decision, you can always alter course. Having a route mapped out doesn’t mean that you have to stick with it. Once your brain tumour has been diagnosed your case should be discussed at a multidisciplinary team meeting (MDT meeting). A key recommendation of the NICE* ‘Improving Outcomes Guidance’ is that:
The care of all patients with brain and other central nervous system (CNS) tumours should be coordinated through a specific model of multidisciplinary assessment and care:
- a designated lead in every acute trust
- a neuroscience brain and other CNS tumours MDT
- a cancer network brain and other CNS tumours MDT
- a key worker
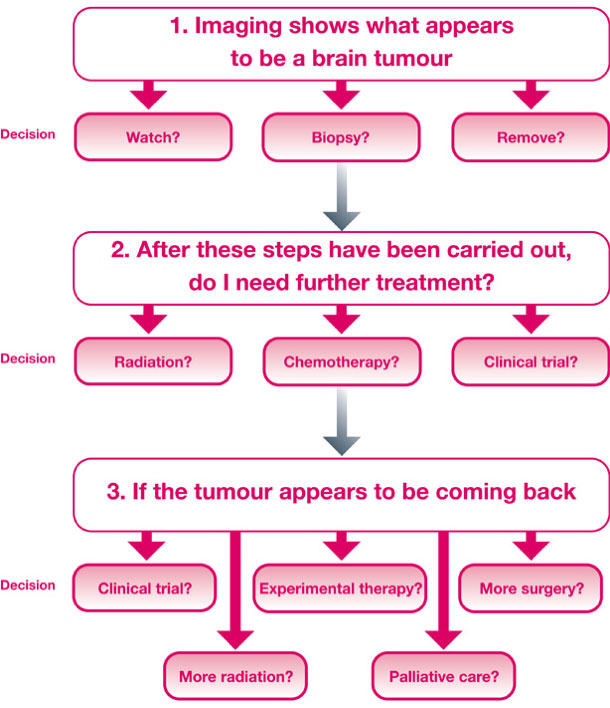
As a number of options will be available for your treatment these meetings are very important and should be the minimum which you can expect. The MDT meeting will enable your case to be discussed by radiologists, neurosurgeons and oncologists. They will the best pathway for you.
Treatments will depend on the type and grade of brain tumour. The most common forms of treatment are:
- Watch and wait
- Surgery
- Drug therapy (chemotherapy, immunotherapy, gene therapy)
- Radiotherapy
- Combined chemo/radiotherapy
- Best supportive care
Your treatment plan will either be radical and/or palliative:
Radical: In some cancers the intent is to cure. For brain tumours the aim is to stabilize the disease with best standard treatment which currently is a combination of radiotherapy and oral chemotherapy.
Palliative: The intent here is to relieve the symptoms when a cure is not possible. Sometimes it is better to look after the symptoms because to deal with the cause may be too damaging.
However, it would be nice to think that you might be included in these decisions too! So these are the things that you should consider, to make sure that your care pathway belongs to you and not the MDT:
- Your wishes regarding your treatment
- The type of tumour
- Where it is located
- The size of tumour
- The risks and potential benefits of available treatment options
- Your overall health
- Your age
- The type of healthcare services available and your ability to travel
- What other options are available outside your locality, even country
| MDT member | Description |
| Neurosurgeon(s) | A specialist neurosurgeon who spends at least 50% of clinical programmed activities in neuro-oncological surgery and is regularly involved in dedicated speciality clinics caring for these patients. |
| Neuroradiologist | A consultant radiologist with at least 50% of clinical programmed activities spent in the practice of neuroradiology. |
| Neuropathologist | Registered as a Neuropathologist or histopathologist and has specialist expertise in neuro-oncology.. |
| Neurologist | A consultant neurologist with expertise in neuro-oncology, epilepsy or neuro-rehabilitation. |
| Oncologist | A clinical oncologist with a special interest in tumours of the CNS |
| Clinical nurse specialist | A nurse with specialist knowledge of CNS tumours and skills in communication |
| Palliative care | A healthcare professional (normally a member of the palliative care team) with experience and expertise in the provision of palliative care services for patients with CNS tumours |
| Neuropsychologist | A clinical neuropsychologist with a special interest in tumours of the CNS |
| Specialist allied health professionals (AHP) | Representative of AHPs, including occupational therapy, physiotherapy, speech and language therapy, dietetics and others as appropriate, who have knowledge and experience of dealing with the patient group, with responsibility for education and liaison with other local AHPs |
| Coordinators | An administrative post responsible for coordinating patient registration with the neuroscience MDT and data collection |
| Others as required | E.g. representatives from ward nursing, community palliative nursing, psychology/psychiatry and epilepsy nurse specialists |
The best practice should look like this, so that you don’t become ‘lost’ in the system:
For more information about some of these professionals have a look at our Who’s Who in Your Clinical Team booklet.
The website you have prepared is impressive and very helpful to many of those struggling with their diagnosis and treatment.
Professor Roy Rampling, Glasgow
Resources used in creating this page:
brainstrust patient/carer representative
Consultant Neurosurgeon
Clinical nurse specialist
National Institute for Health and Clinical Excellence guidelines – Improving Outcomes Guidance Brain and CNS Tumours 2006
Living with a Brain Tumour (Peter Black) 2009
Fast Facts – Brain Tumors (Abrey and Mason) 2009
Primary Central Nervous System Tumors – pathogenesis and therapy (Current Clinical Oncology, Humana Press 2011)
Did this information make you feel more resourced, more confident or more in control?
Date published: 17-05-2009
Last edited: 28-02-2018
Due for review: 28-02-2021
This information is currently being reviewed as of Feb-2022
Subscribe to our mailing list to hear about all the latest news, events, research and resources.
Coaching with brainstrust
Our coaching conversations are about collaboration, we will listen, listen some more, then ask questions. Our support specialists are trained to help you realise what matters most to you and come up with a plan to reach your specific goals.
Finding out about your brain tumour diagnosis leaves you feeling confused, panicked and overwhelmed. Book a coaching session today to start taking control.