I want to hear from others who understand
When you are diagnosed with a meningioma, you may find yourself feeling alone, isolated and lost. This is something that many people feel, regardless of what stage of the pathway they are on. There is real value in being able to speak to others who understand and can relate to what you are experiencing. In this section, we share meningioma patient stories and more information on how you can connect with other people with a meningioma diagnosis and go from feeling isolated to included and part of a community.
Read about other people’s experiences of living with a meningioma
“It does take time to heal from the shock as well. Let alone from the operation itself. Family and friends just see us smiling and up and about like we used to be – they don’t see the internal struggle. Takes time to heal mentally as well physically.”
Read Andy’s story

“When I was ten years old, I learnt that life can change in an instant and it showed me that we have to value our lives because we just don’t know what could happen. When I was just ten years old, my mum was diagnosed with a brain tumor and that suddenly changed everything. This is my story about fighting from the side lines.”
Read Charlotte’s story

“There had to be some explanation for my constant migraines, hands that trembled and an increasing everyday struggle to find words. I constantly forgot things like work assignments, and I would faint flat out on the floor at random times of the day and in public places. I would suddenly be completely blind for a few moments, as though my eyes were tight shut when in fact they were wide open. My symptoms were dramatic, and they were taking their toll. I was scared and depressed.”
Read Claire’s story

“Life may never be the same after the operation, but the key word is LIFE and I am grateful to be here for both myself & for my family and friends. If it’s an altered life going forward, then so be it.”
Read Emma’s story

“The news was delivered to be in a small broom cupboard. The words will always haunt me, “I am sorry but we have found a large mass in your head. We will have to start you on a cocktail of drugs and will not be able to let you go home as we do not know your prognosis”. I took one look at my husband and asked him if he was ok, then said we had better arrange for my sister to stay overnight with the kids.”
Read Jaime’s story

“Thanks to brainstrust, I now feel like I am part of a community and feel comfortable and confident whenever I have needed to ask for help. I stopped feeling lonely and scared, as I now know there is always someone who will help. When you hear the words ‘you have a brain tumour’ your life changes in a split second. Having there has helped me to deal with it, and I will be forever grateful.”
Read Sarah’s story

Meet others who understand.
As well as reading meningioma patient stories, connecting and talking with other people who are also living with a meningioma diagnosis is so important. It can help you feel less alone, and part of a support community. There’s a few different ways you can get involved whether it’s on our Facebook group, at our monthly virtual meeting, or through peer support. Click the link below to find out more about how you can connect with others in the meningioma community.
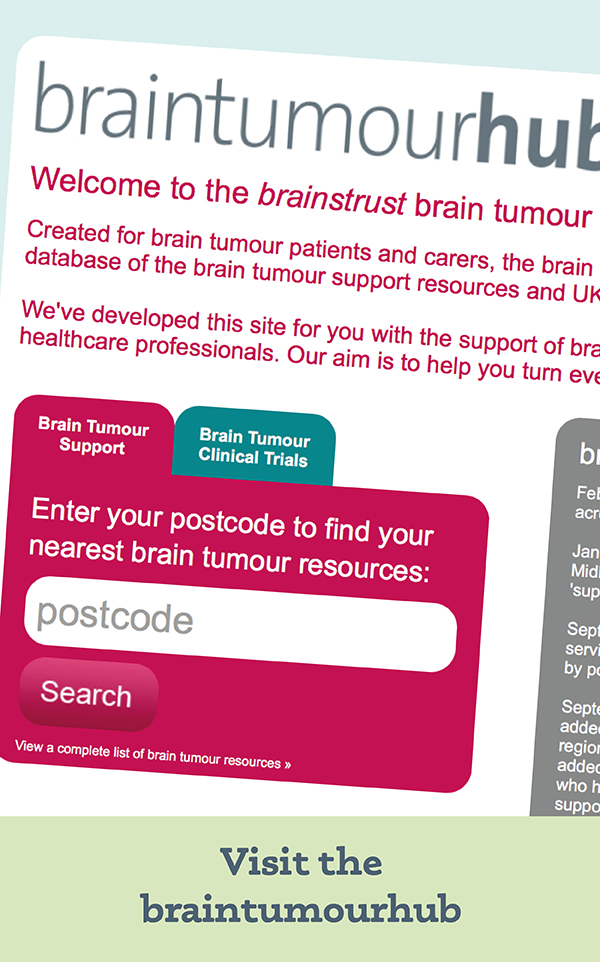
Discover our resources, designed to help you feel less alone and more in control.