Novel treatments and trials for Glioblastoma (GBM)
Here is a list of alternative and novel glioblastoma treatments including immunotherapies, repurposed drugs, checkpoint inhibitors and more. Each treatment has a description of what it does, what research has been done to legitimise it, if it is currently available and general costings.
The information here has come from the community and is for the community. We are not recommending these treatments, just signposting and sharing what information there is so that you can begin to have further conversations. Only you know what your appetite for risk is, what your context is and what your values are. This information will be updated regularly.
We can’t ensure that any of these treatments will be of benefit, but we can save you time searching by sharing this list. We want you to spend your time doing what’s important to you and your loved ones.
If you have any treatments that to suggest for this list, please email adam@brainstrust.org.uk
Working together to help people with a brain tumour
brainstrust and myTomorrows share the commitment to support people with brain tumours, and their families. We know identifying and pursuing a clinical trial can be challenging, and together we provide support on this journey. This support is always free of charge for people with brain tumours and healthcare professionals in the United Kingdom.
Know how to talk with your neurosurgeon about tissue collection. Download the know how.
Current novel treatments and trials for glioblastoma (GBM)
Updated July 2023
Immunotherapy
Although cell therapy is a promising and exciting field, these complex therapies still need to be studied more in depth before they can be administered to a larger population. Patients should not pay for experimental treatments but should be included in clinical studies, where therapy is free of charge. Moreover, these studies should be approved by an ethics committee and be listed in a publicly accessible clinical trial databases, ensuring patients’ rights and safety are guaranteed.
ADCV (DCVax®)
DCVax®-L is an immune therapy made from each patient’s dendritic cells and specific biomarkers (antigens) from their glioblastoma tumour (GBM). Dendritic cells are a type of immune cell that help the body’s immune system recognise and attack potentially harmful things, such as foreign invaders or tumour cells. A marker or element of the invading microbe or pathogen, or the tumour cell, is called an antigen. It is seen as a threat by the immune system and can stimulate an immune response.
Dendritic cells conduct surveillance throughout the body, and when they find an antigen in the body, they alert multiple parts of the immune system to respond, including mobilizing T cells against the antigen and producing antibodies against it. DCVax®-L is composed of a patient’s own dendritic cells. A patient’s immature immune cells are obtained through a blood draw, and then are matured into dendritic cells in a lab, and activated and educated to recognize the antigens from the patient’s own tumour. These dendritic cells are reintroduced into the patient (by a simple injection in the arm, similar to a flu shot) to mobilise the body’s own immune system to attack the GBM tumour. When reintroduced into the body, the DCVax®-L dendritic cell vaccine educates the immune system about which antigens to attack.
NWB has published phase 3 trial results and has opened a production plant in Sawston, Cambridge. This has all the regulatory approvals.
The latest press release for DCVax can be found here.
You can read our comments on the latest news for DCVax here.
Did you can fundraise for brain tumour treatments, like DC-Vax, with brainstrust? Find out more here.
It generally costs £250,000. More information can be found here.
CeGat diagnostics: peptide vaccine
Whilst CeGat is essentially a diagnostic service, offering a comprehensive laboratory expertise, it does also offer a peptide vaccine. From the analysis it can elicit tumour antigen-specific immune responses.
It is not as personalized as ADCV and targets 10 generic peptides. We have several patients who have gone down this route. The choice tends to be made as a second option if ADCV is financially out of reach.
If patients opt to continue beyond the diagnostics, the cost is around £55k. You can fundraise for this with support from brainstrust. Find out more here.
Keytruda
This has been shown to have a significant effect against brain cancer, but only where you have the presence of a tumour. If 98% has been removed, it has no effect. The trial was with just 35 randomised patients and involved 16 using the immunotherapy before and 19 using it after surgery. All patients had recurrent glioblastoma. The study by the Ivy Foundation found that where the tumour had not been removed, the immunotherapy reactivated T-cells in it and these damaged the tumour. If the tumour had been removed through surgery, this effect could not happen.
Patients who used the drug prior to surgery survived on average 417 days; those who used it after, 228 days.
This was a phase 1 trial. No surgeon would give this treatment without further evidence, so this needs to move to a phase 2 trial first.
Ipilimumab
This works by stimulating certain immune cells called T-cells to find and attack the cancer.
It has shown evidenced success in melanoma and kidney as an immunotherapy treatment. Scientific info.
Immucura
This is a clinic in Spain which focuses immunotherapy for a variety of cancers, including brain. Immucura describes its cell-based immunotherapy as ‘the last hope for many cancer patients’. On its website, the clinic mentions the cultivation of monocytes (blood cells) into immune managing cells (dendritic cells) and how to teach them to fight cancer with cancer antigens. This type of medicinal product is called an ATMP (advanced therapy medicinal product) and should comply with the European ATMP regulation.
The specific dendritic cells therapy of Immucura is unregulated and has been confirmed by the Spanish competent authorities. Moreover, the specific therapy seems unproven as there doesn’t appear to be any evidence coming from Immucura in the published literature.
This therapy became a topic of interest recently in Belgium through Goedele Liekens, a public figure, politician and a cancer patient promoting the treatment in the media. As a response, Professor Bart Neyns (Free University of Brussels), who has been conducting research on dendritic cells for years, highlighted the danger of treating patients in a non-controlled environment in the newspaper: “Removing cells, treating them in a lab and reinserting them: all kinds of things can go wrong. If the quality of those dendritic cells is insufficient, they can even signal the body not to reject cancer cells, but on the contrary accept them.“
IOZK Vaccine
IOZK therapy, offered by the Immune-Oncological Centre Cologne (IOZK) in Germany, is an advanced personalised treatment. It combines several immunotherapy techniques to enhance the body’s natural ability to fight cancer.
The key components of IOZK therapy include:
- Oncolytic Virotherapy: A virus, typically the Newcastle Disease Virus (NDV), is used to infect and destroy cancer cells. This virus also activates the immune system, helping it to recognise and attack the tumour.
- Dendritic Cell Vaccine (IO-VAC): This personalised vaccine is created using the patient’s own tumour material and dendritic cells. It stimulates the immune system to specifically target and destroy cancer cells.
- Hyperthermia: The therapy involves using controlled heat (electrohyperthermia) to stress and weaken tumour cells, making them more susceptible to immune attacks and increasing the effectiveness of other treatments.
- Checkpoint Inhibitors: These drugs help to “unblock” the immune system, allowing it to continue fighting cancer cells that would otherwise escape immune detection.
The entire treatment plan is highly individualised, starting with a detailed analysis of the patient’s tumour and immune system. The therapy typically takes around five weeks for the initial phase, with costs for the first two treatment cycles starting at around €55,000. Some private insurance providers may cover part of the cost. Patients interested in IOZK therapy typically need to travel to Cologne, Germany, where they can undergo a comprehensive assessment and have their personalised treatment plan developed.
You can find out more on the IOZK site.
Transforming Glioblastoma Treatment: Individualised Multimodal Immunotherapy Explained – Dr Van Gool
IMI integrates multiple therapeutic modalities to address the complexities of GBM. In addition to neurosurgery and radiochemotherapy, IMI includes immunogenic cell death therapy, which involves oncolytic virus therapy and modulated electrohyperthermia. These therapies aim to release danger signals within the tumour microenvironment, triggering an immune response. Following these treatments, active specific immunotherapy, using dendritic cell vaccines, is administered to stimulate the patient’s immune system to recognize and attack the tumour.
IMI has shown promising results in clinical trials. For patients with IDH1 wild-type, MGMT promoter-unmethylated GBM, combining chemotherapy with IMI extended the median overall survival to 22 months, with a two-year survival rate of 36%. For IDH1 wild-type, MGMT promoter-methylated patients, the combination treatment resulted in a median overall survival of 33 months and a two-year survival rate of 82%.
Dr Van Gool joined us in an expert-led webinar, which you can watch below
In this video, Dr Van Gool discusses:
- The challenges of treating glioblastoma and its ever-changing nature.
- The limitations of current standard treatments, including surgery, radiotherapy, and chemotherapy.
- How innovative therapies like immunogenic cell death (ICD) treatment, dendritic cell vaccines, and tumour-specific immunotherapies can improve outcomes.
- Real-world data demonstrating significantly better survival rates with immunotherapy.
- Practical and ethical considerations for incorporating personalised immunotherapy into cancer care.
Whether you are a patient, carer, or medical professional, this video offers valuable insights into the future of glioblastoma treatment and the potential of personalised medicine.
A transcript of this webinar is also available for download here
Find Out More:
For additional details about Individualised Multimodal Immunotherapy or to explore treatment options, visit the IOZK website: https://www.iozk.de
Contact: info@iozk.de
Repurposed Drugs
Repurposed drugs have shown in laboratory experiments to maybe have an effect but to date no trials have shown a survival benefit. It would be hard for these to go to trial as these drugs are cheaply available in the market place and so therefore there is no attraction to pharma.
Metformin
Metformin hydrochloride may stop the growth of cancer cells by blocking some of the enzymes needed for cell growth.
Metformin has been linked to improve survival of patients with various cancers. There is little information on survival of glioblastoma patients after use of metformin. Assessment of the association between metformin use and survival in a pooled analysis of patient data from 1,731 individuals from the randomized AVAglio, CENTRIC and CORE trials showed that Metformin did not prolong survival of patients with newly diagnosed glioblastoma in the analysis. Additional studies may identify patients with specific tumor characteristics that are associated with potential benefit from treatment with metformin, possibly due to metabolic vulnerabilities.
Prices vary according to medication but largely are not expensive.
METRICS
These medications (metformin, atorvastatin, mebendazole, and doxycycline) modulate pathways involved in cancer cell growth. The combination of medicines used in METRICS was chosen following an analysis of existing mechanistic and clinical data. The protocol for Glioma can be found here.
The Care Oncology Clinic (COC) in London prescribed METRICS so you may hear some people talking about it. The COC was part of a US based organisation. However, the COC has closed down and is no longer operational. There is a new clinic opening but it would appear to have a different focus.
Questions to consider when approaching clinics like this are:
- What therapies do they recommend for brain tumours? It would be a concern if there is no specific reference to brain tumours.
- What evidence is shared that shows the therapies are efficacious for brain tumours?
- Are the clinicians registered with a professional body?
As ever, always talk with your clinical team. If you are on the NHS standard protocol (Stupp) then some additional therapies can counter chemotherapy and radiotherapy.
Low Dose Naltrexone (LDN)
Works as an anti-inflammatory, modifies certain genes and promotes cancer cell death and enhances the immune response greatly. It stimulates the immune response. This allows LDN to be used along-side conventional cancer-cell killing agents. Here is more scientific information.
The initial consultation costs £165 with a monthly membership fee of £62.50 thereafter and is available at the Harpal Clinic, London.
For prescribers see The LDN Trust.
Sertraline
Sertraline helps to inhibit the growth of cancer cells. Its potential lies in the fact that it passes the blood brain barrier. It is also used as an anti-depressant.
The safety of using sertraline in humans has already been well described, which is a great advantage. Studies performed at American Association for Cancer Research. Here is more Scientific information.
Cannabinoids
Cancer cells have signal pathways which control growth. CBD alters the signal pathways to affect cancer growth. Both THC and CBD have been proved in the laboratory to alter these signal pathways.
A small trial of 6 people has shown some efficacy; a larger phase 2 trial (Aristocrat) is due to open in 2022. Patients need medical grade cannabinoid produced by Sativex.
Cost varies depending on pharmacy but about £400 per pack of 270 doses. To receive this treatment, try to discuss with a consultant neurologist.
Here is Cannabinoids – information for patients and carers.
More information at GW Pharma Ltd.
Antivirals
Oncolytic virotherapy (OVT) is a unique anti-tumour immunotherapy wherein viruses selectively or preferentially kill tumour cells, replicate and spread through tumours while inducing antitumor immune responses. OVTs can also recondition the tumour microenvironment and improve the efficacy of other immunotherapies by escalating the infiltration of immune cells into tumours. Scientific overview here.
Pelareorep (Oncolytic Virus)
Pelareorep can kill cancer cells. Here are some positive results from a trial. Concluded that pelareorep might be a useful treatment for GBM, for some. Trial completed in 2019. Results reported 2020.Trial has ended. It was carried out at the University of Leeds and patients must not have had treatment other than surgery.
Delytact
This is the first OV that has been approved for brain cancer but only in Japan. Delytact, which was jointly developed by Daiichi Sankyo and the University of Tokyo’s Institute of Medical Science , is a triple-mutated, replication-conditional herpes simplex virus type 1 (HSV-1) that has been developed to replicate only in cancer cells. These engineered viruses also referred to as oncolytic immunotherapy can selectively replicate in tumour cells until cell death, after which more viruses are released to target more tumour cells.
This decision was based on a phase 2 study were patients with recurrent GBM met the primary endpoint of one year survival rate. Press release from pharma.
This is not available in the UK. For the time being, DELYTACT® will be commercially available only at hospitals that served as trial sites. Daiichi Sankyo will establish a stable supply system of the medicine as soon as possible.
Reovirus
Reovirus occurs naturally and can cause a mild fever in children. But once the reovirus enters a cancer cell, it replicates and destroys it, generating chemical signals in the process that stimulate the body’s own defence mechanisms to attack the cancer.
Nine patients took part in the study. They had cancers that had either spread to the brain from other parts of the body or were fast-growing gliomas, a type of brain cancers that is difficult to treat, and has a poor prognosis. All patients were due to have the tumours removed surgically. But in the days before the surgeons operated, the patients were given the virus drip.
Once the tumours were removed, samples were taken and analysed for signs that the virus had been able to reach the cancer, sometimes deep within the brain. In all nine patients, there was evidence that the virus had reached its target.
Bottom line – this is not a treatment but a method for getting drugs to target.
This trial set out to see if the virus could cross the BBB and reach its target. The study authors, from the University of Leeds and The Institute of Cancer Research, London, believe reovirus therapy could be used in conjunction with other cancer therapies to make them more potent. Up to now, scientists thought it was unlikely that the virus would be able to pass from the blood into the brain because of the blood-brain barrier, a protective membrane around the brain. That would have meant that the only way they could get the virus into the brain was to inject it directly – which is challenging, would not be suitable for all patients, and cannot easily be regularly repeated.
The findings, published in the journal Science Translational Medicine, demonstrated that the virus could be administered through a single-dose intravenous drip.
Angiogenetic drugs
Bevacizumab (Avastin)
Bevacizumab is an angiogenetic drug. This means that it reduces the blood supply to the tumour. Initially in early trials this was seen to be reducing the tumour size but then clinicians realised it was masking growth as they thought scans showed a reduction in tumour size, but it was actually the blood supply. It is also thought that it can cause further tumours and brain bleeds.
Multiple studies of the humanized vascular endothelial growth factor (VEGF) antibody bevacizumab for glioblastoma have failed to demonstrate a survival benefit. However, bevacizumab is often effective in reducing oedema and related clinical symptoms and signs. It is approved in the United States and some other countries, but not in the European Union or the UK, for use in recurrent glioblastoma due to improvement in progression-free survival (PFS) and reduction in corticosteroid use. Continuation of bevacizumab post progression did not improve outcome in a small study. Patients with recurrent glioblastoma should ideally be considered for clinical trials before receiving bevacizumab, as most trials exclude prior use of bevacizumab. Bevacizumab has also been proven to be effective in radiation-induced necrosis, although the doses used are lower than standard dosing for recurrent glioblastoma (typically 7.5 mg/kg every 3 wk for a maximum of 4 treatments).
It is not available on the NHS in the UK due to lack of evidence and cost but some insurers will fund it. Usually patients have to go to appeal at a time when there isn’t much time (they are at recurrence) and are heightened emotionally.
Early phase trials, so no market access
These are potential treatments which have or are undergoing early phase or phase 1 trials, so in the lab or in very small cohorts of patients (less than 10).
Lisavanbulin and glioblastoma (GBM)
Personalised medicine is recognised to be the best way to treat cancers, not just brain cancer. This means that treatments are created and targeted to treat the molecular make up of cancer. The exciting news about lisavanbulin is that this could potentially be one of the first targeted treatments for glioblastoma, the most aggressive form of brain cancer, when it recurs.
And herein lies the problem. The brain is a delicate and privileged site and brain tumours are complex, rare and intrinsically resistant diseases. We know that when a GBM tumour recurs, it is not the same as initial disease. We know too that individual treatment agents in isolation are doomed to failure, because there are multiple growth pathways that must be inhibited simultaneously. In other words, the cancer cells keep finding ways to work around the treatment.
So how is lisavanbulin having an impact? lisavanbulin is a produced by Basilea Pharmaceutica Ltd, a biopharmaceutical company based in Switzerland. Data from GBM mouse models and recent phase 1 clinical data (Lopez et al. ESMO 2020) suggest that EB1 is a response-predictive marker for lisavanbulin in GBM. This means that GBM tumours with the molecular marker EB1 may respond to lisavanbulin. A phase 2 study is ongoing at The Royal Marsden to confirm this hypothesis. So far two patients have shown a positive response.
It is very early days and as ever with personalised medicine, it will only be meaningful for small cohorts of patients who have the predictive marker, in this case EB1. The reason this has made the headlines now is that the results were reported recently at The American Society of Clinical Oncology conference (ASCO).
So potentially yes – this may be a game changer. But – it is a long long way from coming to to the clinic and if it does, then it will only be suitable for a very small cohort of patients who have the EB1 predictive marker. We need to see the results for the phase 2 study. If these show promise then phase 3 and phase 4 studies will follow. At this point, if it is proven to be successful, the treatment will need to be approved by the National Institute for Health and Clinical Excellence so that it can be provided by the NHS. This too would mean a change in the way tumours are tested, as the GBM tissue will need to be tested for the EB1 predictive marker.
The bottom line? Yes, lisavanbulin shows promise in the lab with mouse models and currently in just two patients. But we have so many hurdles to cross before it could potentially be used in the clinic. This will take years and of course, may fall at any of the hurdles, like so many other potential treatments have to date. So whilst partially accurate, our feeling is that this reporting builds false hope. Clinicians are not able to prescribe this treatment at the moment and they may never be able to. You can though access it through signing up to the trial.
If you want to find out more then there is more information here. The Royal Marsden in London and The Beatson in Glasgow are currently recruiting to be followed by University College London, and the Sir Bobby Robson Cancer Trials Research Centre; Northern Centre for Cancer Care in Newcastle. Do have a look at the inclusion and exclusion criteria – these are very stringent and of course, it is only appropriate for people who have the predictive marker EB1.
Ice-Cap trial
Ice-Cap was a phase 1 trial involving ten patients run at the Royal Marsden. Two of the first 10 patients treated for glioblastoma on the trial responded to the immunotherapy drug atezolizumab in combination with ipatasertib, a new precision drug. It was particularly effective for patients with defects in the PTEN gene.
So this means that firstly the patient would have to have defects with the PTEN gene, and only 20% showed a response so it is a very limiting treatment. This would now need to go to a phase 2 trial so this would be the only way patients would be able access this treatment. It is not yet at this stage.
And we had advice from Juanita Lopez – the principle investigator who is leading on this:
We are just writing up the manuscript now. The Phase 1 data is quite exciting where we did have some exceptional responders with complete PTEN loss, and on the back of that Roche was keen to fund an international Phase 3 randomised trial. We were fairly far down the road working on this, when the same drug combination failed to meet the endopoints in first a Phase 3 breast trial and then a Phase 3 prostate trial. So the current status is that any further development of the drug is halted, we are hoping that if we get the manuscript published in a high impact journal, we can then persuade pharma to allow us to undertake a further trial.
Arginine
So this is work that has been done at Imperial and with all of these things that might show promise in the lab, it is still early phase and not in an in-human trial at the moment. And we know from previous research that, whilst mouse models are the closest model to the human brain, the research does not translate well. It will be years before this is developed into a phase 1 trial and then, as with all the other trials, will probably fail. More reading can be done here, but as this is published scientific research it will of course not include a commentary on what this means for the person with the lived disease so it sounds positive but is far removed from reaching the clinic. Additional article: https://www.jci.org/articles/view/142137#SEC3
If people want more info I would suggest they email Nel (Nelofer), but it won’t change any treatment pathway at the moment as this isn’t available. Nel can be emailed on n.syed@imperial.ac.uk.
Selinexor
Selinexor causes cell cycle arrest and death in cancer cells.
It has undergone a phase 2 trial for recurrent GBM and the results were published in February 2022. It would need now to go to a phase 3 trial where a larger cohort of patients can be utliised.
It wasn’t well tolerated with over a third of patients (34.2%) having a serious adverse event. It isn’t available as a treatment. No NHS clinician would prescribe this outwith a trial. More info here.
Auceliciclib
Auceliciclib has demonstrated in pre-clinical models that it can cross the blood-brain barrier, which makes it an ideal drug candidate for brain cancer. It has two key advantages over other drugs in development. It is more target-specific, reaching cancer cells in the brain more effectively, and is less toxic.
This is a very early phase trial – it is a phase 1a/b which means that it hasn’t yet been tested as an in person trial – it has been done in the lab with mice. It will be a very small cohort of patients to start with to see how successful it is. If it meets the endpoints then it will go to a phase 2 trial and be tested on a larger volume of patients. To access Auceliciclib you would need to be living in Australia and being treated at one of the two centres that is running this trial. More info here: https://www.aucentra.com/clinical-trials/
Technology
Novocure Tumour Treating Fields (Optune, technology)
This is a skullcap like device with stimulating patches within. It uses alternating electrical fields to disrupt tumour cell division, or cause cell death, thereby preventing the tumour from growing or spreading so quickly. It uses alternating electrical fields to disrupt tumour cell division, or cause cell death, thereby preventing the tumour from growing or spreading so quickly.
It is Novocure’s goal for it to have market access for this through the NHS but currently it doesn’t pass the health economic test with numbers of years of life lost v costs. We have several patients who are using it, but considerations come into play. More info here.
Optune can cost in the region of £17,500 per month. Some insurers will cover this; some won’t.
Not currently available on the NHS, some oncologists can prescribe it privately. For more information about how to access this technology please email support@novocure.com.
Should you want to, you can fundraise for TTF technology with support from brainstrust. Find out more here.
Other
Sugar Bomb (Preclinical)
Scientists found that combining the tiny bacteria-killing molecule with a chemical food compound can trick bacteria into ingesting the drug, avoiding the chances of attacking healthy tissue and preventing the kind of side effects caused by other drugs.
Researchers say further tests are needed to show if the drug is a safe and quick method of treating early-stage cancers and drug-resistant bacteria.
Studies are being carried out at the University of Edinburgh. This is not currently available to the public.
Sonalasense (Drugs and Ultrasound)
Aminolevulinic acid (ALA) sonodynamic therapy (SDT) is created through the union of two FDA-approved technologies: ALA tumour targeting and focused ultrasound (FUS). This is FDA-approved for the non-invasive treatment of essential tremors as well as those arising from Parkinson’s disease.
Find out more about Sonalasense here.
Intra-ommaya oncolytic virotherapy
Read about this treatment via our Youtube video, with a talk from Dr. Beni Gesundheit.
More resources to help you take control following a Glioblastoma diagnosis
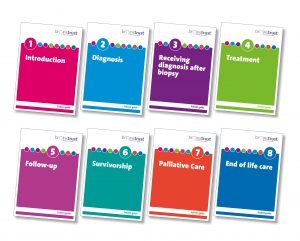 Brain tumour patient guides to let you know what care to expect as a brain tumour patient.
Brain tumour patient guides to let you know what care to expect as a brain tumour patient.
Information about common treatments (surgeries and therapies).
Support to live well with a brain tumour.
Practical help for living with a brain tumour.
For help with taking control.
Support for those caring for someone who has a GBM?
Feel less alone and more informed with webinars and meetups
Our online events include the GBM group, calmness and connectivity webinar, educational talks from professionals, information on treatments such as cannabinoids and guide you to managing new behavioural changes.
Click here to look at all of our upcoming events.
More support, and getting involved in research
Do you want to help support research? Take a look at our PRIME page.
If you have been affected by a brain tumour diagnosis, please reach out to us by calling 01983 292 405, visit our support page or email hello@brainstrust.org.uk
brainstrust relies on donations in order to provide vital support for people with brain tumour. Fundraise to support this work.
Subscribe to our mailing list to hear about all the latest news, events, research and resources.
Coaching with brainstrust
When you’re making treatment decisions it’s important that you know your values and priorities. As coaches we can help you understand what’s important to you, and use this to help you create a plan to reach specific goals.