Hi there! I’m Laura, brainstrust’s Support Specialist for the Central Southern region of England and I work from my home in West Sussex. I like to get out and about and attend events in the local community as often as I can, whether that’s running a workshop or waving the brainstrust flag at an exciting fundraising event. I hope that we have crossed paths or will do soon, whether it be virtually or in person.
Join me below as I talk you through what a day as Laura at brainstrust can look like:
*Names and personal details have been changed to protect the privacy of individuals.

My sun spot for my morning coffee
8am
After having got myself ready for the day, I head down to the kitchen to make myself a frothy coffee. I sit outside in my favourite morning sunspot to read and listen to the birds. I find that this is the perfect way to prepare myself for the day.
9am
I sit down at my desk and head straight for my emails. I spend the first hour of the day responding to emails from patients, caregivers and healthcare professionals. At the same time, I gradually add to my to do list for today.
I then prepare for my coaching call with Dani*. Dani was diagnosed with a meningioma tumour last year and today will be our third coaching session together.

My work from home set up
10am: Coaching call with Dani
Our coaching call today picked up on where we left off last week. In our first call together, Dani and I created a “wheel of life”, which is a coaching strategy aiming to map out all the areas of life most important to you and encourages the you to rate how satisfied you are in each area. Dani decided to label one section of her wheel of life “me time”. For Dani, “me time” encompasses activities that she does for fun and things that she does for self-care. As a busy parent of three and having had an awake craniotomy 6 months ago, Dani has found that she has less and less “me time” and rated this area as 2/10 for satisfaction.
After exploring this together, Dani decided to speak to her partner about the importance of having this time and we have worked together to identify pockets of time in Dani’s week that she can dedicate to these activities. Following our second session, Dani wanted to give hypnotherapy sessions a go to find a way to relax and de-stress during her week. Following our third session today, Dani has started to create a list of “me time” activities and will be putting these in order of which ones she would like to make time for first. Hypnotherapy is top of the list and she will be joining the evening session at 7pm tonight (as will I!)
11:30am: Follow the Seagulls meeting
My colleague, Molly, and I are facilitating brainstrust’s first Follow the Seagulls walk in Brighton this June. I join the meeting with my colleague, Steph, in the fundraising team and Will, our CEO, to chat through logistics and check that we have everything we need to support our walkers. They will be taking on 50 miles, split over two days – it is a huge challenge! They are incredible to take this on and we will be there to cheer them along every step of the way.

Company for my lunch time walk
12:15pm: Lunch time
As the sun is shining, I decide to walk through the woods and sit by the river behind the house. It is so peaceful here and a perfect lunch spot.
1pm: Peer support volunteers’ monthly Zoom call
One of my favourite parts of my role is nurturing and growing our peer support service. Our peer support volunteers are an incredibly inspiring and resilient group of patients and caregivers who have a wide range of lived experiences and regularly connect with members of our community, helping them to feel less alone.
We meet once a month to check in. Our peer supporters have the chance to debrief and discuss recent peer support calls that they have had. To start the call, we always have a “skills training” segment to help them feel confident in their peer support role. Most recently, we have been focusing on active listening skills. We run through some training together and have a chance for group discussion.
During the group discussion today, one of the peer supporters, Kian*, who has joined the peer support volunteer team more recently, raises that he is yet to have been matched with a supportee. All of our peer supporters understand that demand for our peer support service does ebb and flow, but I make sure to promote our peer supporters to the community. I thank Kian for raising this and make a mental note to flag Kian’s availability to the support team. Kian is supporting his spouse, Fleur*, who was diagnosed with a Grade 2 glioma 2 years ago.
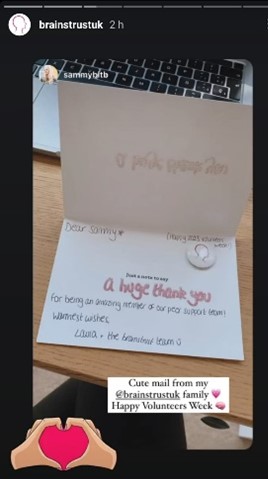
Our volunteers receiving their thank you cards
This week also happens to be Volunteers’ week, so I extend a big thank you to our peer support volunteers. Yesterday, I wrote and posted a card to each of them to thank them from the team for their amazing volunteer work.
their amazing volunteer work.
2:00pm
The brainstrust phone line rings, and I pick up. I introduce myself to and start speaking with Viktor*. Viktor explains that two months ago, his wife had a sudden seizure, was rushed to A&E and scans identified a tumour in her brain. They have been told that the tumour is likely a Grade 2 Glioma, but a biopsy following upcoming surgery will confirm further details. A healthcare professional at the hospital recommended calling brainstrust in the run up to a surgery date.
Viktor shares that he feels that he is not coping and this all feels like a whirlwind. Viktor’s wife had her first seizure just a month after their wedding. I give Viktor space to share how he is feeling and to breathe, empathising and normalising how he is feeling. I ask Viktor questions such as “What are you struggling with the most right now?” and “What feels like the main priority?” I then outline the support that he, his wife and their loved ones can access with brainstrust.
For Viktor, the top priority is helping his wife to prepare for surgery and then supporting her during recovery, he feels that speaking to a caregiver who has been a similar boat would be helpful. We speak more about the peer support service together and how this works.
I explain to Viktor that the brainstrust team works regionally and ask where he is based. I let him know that I will ask my colleague covering this area, Rosie, to reach out and say hello to him.
2:50pm
I know exactly which peer support volunteer to contact… I send Kian an email to ask if he is available to connect with another caregiver in the community. Once Kian has confirmed that he is happy to go ahead, I will share a bit more detail with Kian about Viktor’s situation and introduce them to each other via an email.
3:15pm
I call a patient, Saskia* to triage for our counselling service. Saskia has been referred to me by the Genesis Care Oxford team. To make sure that counselling is a good fit, we always discuss with our community what they want to discuss in counselling and their expectations for the service. Saskia has been experiencing low mood and stress following her diagnosis. Life changes such as losing her driving licence have caused a significant shift in how Saskia lives her life, and she finds herself withdrawing. She feels that counselling would help her to process these and find a way to move forwards and feel more herself again. We agree together that counselling does sound like a good fit. I thank Saskia for her time, then send her the counselling referral forms for us to progress her referral.
4pm
I spend my last hour returning to my emails. I then work my way through the final items on my to do list for today. Finally, I look at my project planning for the month and familiarise myself with priorities and upcoming tasks.
5pm
At 5pm, it is time for a break. I usually finish for the day at 5pm, but today I am facilitating something very exciting at 7pm…
6:50pm: Hypnotherapy Part 1 session
This evening, I am facilitating a Hypnotherapy session. brainstrust, works with Louise Baker, a fantastic, qualified hypnotherapist. Louise helps our community learn strategies to help them relax and de-stress. This session is an introduction to what hypnotherapy is and is a space to learn the techniques together. Once someone has completed a Part 1 and Part 2 session, they are welcome to join Louise’s “weekly reset” sessions. The reset sessions are an opportunity to practice their skills and have a relaxing guided session by Louise.
We have 10 people joining us this evening. I smile and wave when Dani joins the call. I make a note of everyone’s attendance and Louise starts the session.
8pm
I feel so zen and relaxed. Joining these hypnotherapy sessions is definitely a highlight of my job!
Despite working remotely, I feel connected and close with my brainstrust colleagues, which is testament to the importance of joint working and collaboration in the team. I am part of the support team, which is made up of 7 of us dotted around the UK. I joined the fantastic brainstrust team last September and enjoy how varied and unpredictable my work days can be. We’re always working on innovative projects to ensure we are reaching people when they need us and addressing what is most important to them. Our community is at the core of everything that we do.










