World Hospice and Palliative Care Day
This Palliative Care Day, we’re exploring what exactly palliative care is, what it isn’t, and how it fits in with best supportive care?
What is palliative care?
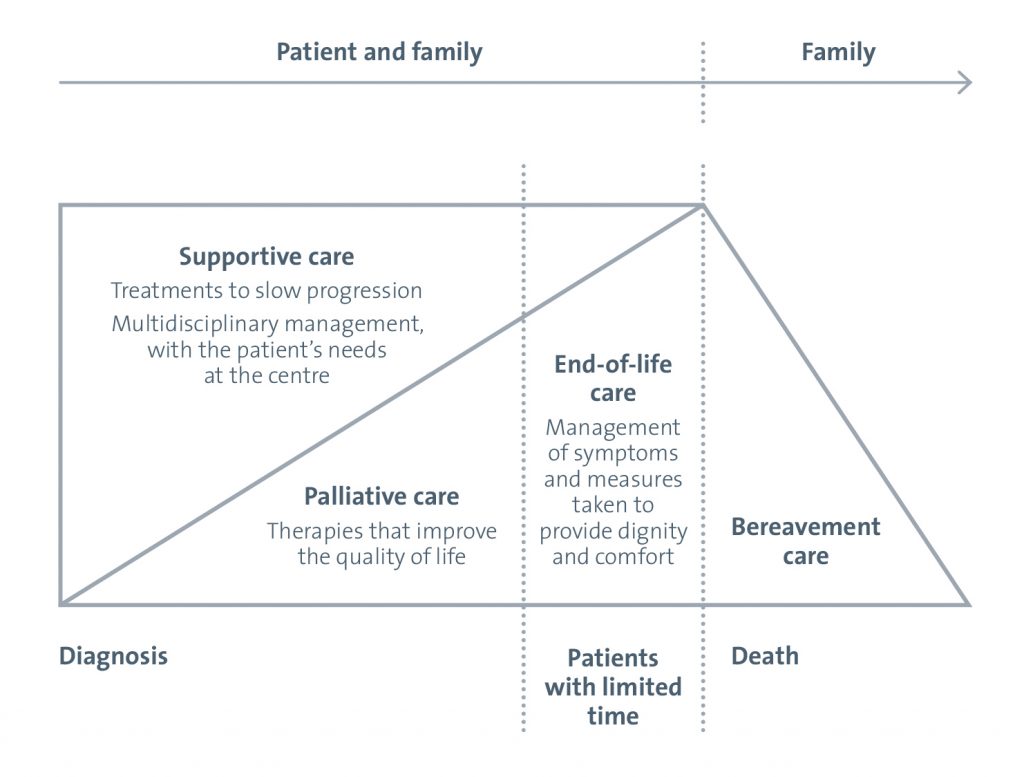
The language used to describe the different phases of the brain tumour pathway can be confusing. Traditionally the words palliative care have been linked to end-of-life. This is because in the 1960s, hospice and palliative care became of age, often established outside mainstream acute care and so the primary focus of palliative care was end-of-life. And this has stuck.
Palliative care
The aim of palliative care is to getting you as comfortable as possible, when you have an illness that cannot be cured. This is achieved by managing your pain, as well as providing psychological and social support for you, your family and any caregivers.
 End-of-life care
End-of-life care
Good end-of-life care helps you to live as well as possible in the months and years leading up to death, as well as and to die with dignity, with your wishes met.
Need to know more about end-of-life care? Click here to find out about our new resource.
In the last 60 years things have shifted; whilst palliative care and cancer care remain separate, we now know that integrated care produces the best results, where the focus is centred on the person living with cancer and their families.
Supportive care
The best approach is one where all the needs of the patient and their family are met for the whole pathway – from diagnosis through to end-of-life. We’d call this supportive care. This means that the starting point is at diagnosis and the focus is on improving quality of life with the patient very much at the centre. So improvement of function, the best symptom management, active use of resources and family involvement throughout become cornerstones of the pathway, all guided by the patient’s needs. This means that interventions are seen as a positive sign.
An example: Speech and language therapy
A brain tumour can cause communication deficits, which become worse with progression. The earlier speech and language deficit is supported, and if the family knows that communication is going to become harder, then everyone has time to say and write the things that are important to them. If this is left to palliative or end-of-life care, it may be too late.
In summary – supportive care is care that begins at diagnosis and an approach that is multiagency, with the patient and their family very much at the centre. The aim of best supportive care is to help you to have a good quality of life so that you can have your best possible day. This includes being as well and active as possible through the brain tumour pathway. It should be based on a person’s needs, and not their prognosis. It can involve:
- managing physical symptoms, such as pain
- emotional, spiritual and psychological support
- social care, including help with things like washing, dressing and eating
- support for your family and friends.
Palliative care does not mean end-of-life
You can receive best supportive care at any stage in your illness. It doesn’t mean that you are at end-of-life – some people receive best supportive care for years. You can also have best supportive care alongside treatments, therapies and medicines aimed at controlling your illness, such as chemotherapy or radiotherapy.