The magic of the ordinary . . .
We know from our daily interactions with you that after a brain tumour diagnosis the sentiments expressed more than anything else are the threat to way of life, lack of behaviour controls, impact on relationships, loss of identity, systemic problems leading to isolation.
We know too that all things brain cancer have been the Cinderella of the oncology world, for many reasons, not just financial. For example, brain tumours are a complex disease with complex biology. The brain is delicate and privileged site that doesn’t respond well to interference. We have a small research community that has struggled to find anything transformative in the treatment of brain cancer. It’s an unlikely career choice for future medics; subspecialty training needs invigorating. And the small cohorts of patients mean that research is hard to do.
Tessa Jowell’s legacy
2018 has seen significant progress addressing these challenges, and it is important to note the influence that the late Dame Tessa Jowell has had on driving change and laying the foundations for a new brain tumour landscape in the UK.
Inspired and catalysed by the sad news of Tessa Jowell’s death from glioblastoma (and aggressive and as yet uncurable form of brain tumour) in May 2018, much is changing in the brain tumour research landscape. This is not about more of the same; we need to do things differently, be disruptive and challenging if we’re to reap the benefits of this one chance to get things right. We will ensure that the community’s voice is in the DNA of the TJBCM.
So it is with some excitement, intrepidation and relief that at last we have an opportunity to put this right. And this is down to the legacy of Tessa, and her amazing daughter Jess Mills. Jess has eloquently reflected on the experience she’s been through with her mum and explains the need ‘to re-establish the ‘magic of the ordinary’- to enable patients and families to live with a sense of peace and assurance that their most loved one are getting the best possible care.’
We now have committed Government funding invested through the NIHR, and with financial commitment from CRUK, and with the right focus and the right people on board, we should at last see traction in treating this horrible disease.
So what is the TJBCM?
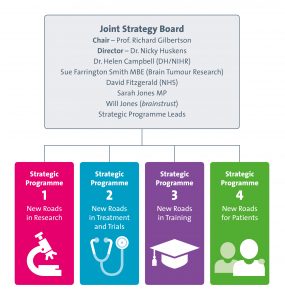
The TJBCM serves as a national convening body, uniting professional, patient, charity and government groups to share information and work together to eradicate brain tumours. The mission puts patients first and foremost, and its aim is to selflessly share insights, knowledge and resources.
We are privileged to be integral to the TJBCM, which means that we can keep you, the patient and the carer, central. We are inspired by you. This is because you are very engaged with the challenges that we all face. You are powerful, vocal force that is happy to support what’s right and challenge what’s wrong with the brain tumour landscape, and as a movement, you are effective in solving the problems we face.
Proof of this can be found in the evolution of the charity landscape in recent years. A nation of people who have been touched by brain cancer has been mobilised to make the world better for people with a brain tumour in the future, and the brain tumour charities are the conduit for this change.
We want each of the 60,000 people who are living with a brain tumour in the UK, and their caregivers, to have parity of care which is second to none, so that there is never any doubt in anyone’s mind that what they are experiencing is the best it can be. We want everyone to know the magic of the ordinary.
You can read more about what the TJBCM means for the brain tumour community here:
https://brainstrust.org.uk/inspiration-from-the-bbc-what-does-this-mean-for-you-part-2/










