Wow. You did it. You definitely were not benign about brain tumours on 1st October 2013.

So the dust is beginning to settle after ‘Wear Grey for a Day 2013’ and we’re able to report the following:
- An estimated 10,000 people took part
- Over £7,000 has been raised so far. This means brainstrust can do even more to help. We will continue to lead the way in helping brain tumour patients and carers solve real, every day issues.
- 14,000 stickers were stuck
- 5,000 flyers flew
- Tons of incredible photos! Click here for just some of them
All of this was thanks to Shaun Skinner and the incredible work of our community of supporters. In fact I think we will start calling you all Angels instead.
Unprecedented engagement
 So Angels, because of your tenacity, your connections and your hardwork, we saw an unprecendented engagement with people, schools, universities, celebrities and businesses.
So Angels, because of your tenacity, your connections and your hardwork, we saw an unprecendented engagement with people, schools, universities, celebrities and businesses.
You really got the word out there.
Hopefully all of these relationships can be fostered in months and years to come, so we can all continue to grow Wear Grey for a Day to raise awareness of, and solve the real problems that burden people battling a brain tumour.
We’ve also been blown away to hear that people wore grey in Australia, New Zealand, Malaysia, Singapore, South Africa, Morocco, Nigeria, France, Netherlands, Norway, Sweden, USA, Canada, Ireland, Italy, Gibraltar and Dubai. You took Wear Grey global!
So in short – THANK YOU SO MUCH for helping us let the world know that every brain tumour diagnosis has an impact.
And that just because all might look ok on the outside, doesn’t mean to say that someone battling the disease isn’t having a tough time. We will continue to monitor brain tumour patient and carer feedback over on our pinboard at www.braintumourawareness.org.uk and hopefully all your work in 2013 will mean that in 2014 fewer people are reporting that they feel ignored, and isolated, and the use of the word ‘benign’ will change.
Building communities on the day we wore grey
 We spent the evening of 1st October at Meet Ups across the UK. We were in Glasgow, Sheffield, London and Cardiff. This is the first time we’ve run the events concurrently – and what a success it was.
We spent the evening of 1st October at Meet Ups across the UK. We were in Glasgow, Sheffield, London and Cardiff. This is the first time we’ve run the events concurrently – and what a success it was.
Over 80 people from these incredible communities got together for conversation and lots of laughs and hugs. And all wearing grey, of course.
The Meet Ups offered brain tumour patients, their carers and clinicians the chance to get together in an informal environment, to share experiences and to meet others in the same boat. We know how isolating things can get and how much you can learn from one another – the true experts. To join in with future Meet Ups, register on www.meetup.com/brainstrust
You are an Angel. 3 tips to make the world better for brain tumour patients.
Whilst only time will tell whether the world is a better place for brain tumour patients and their carers as a result of your hard work on 1st October, we have some simple tips to help make things better in the short term.
If you meet someone who is battling a brain tumour, either patient or carer remember these simple things: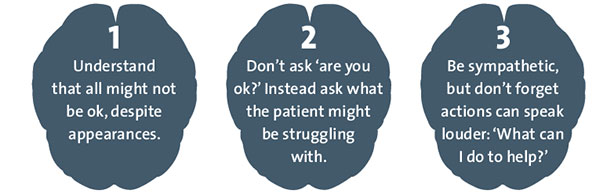
![]() Your Photos – Wear Grey 2013
Your Photos – Wear Grey 2013
And finally, just some of the pictures that were shared during the day on 1st October:



















