After suffering with migraines for years, Kay was diagnosed with a large Meningioma and had to undergo surgery. Kay has written about her experiences from diagnosis, through to surgery and recovery. Below we share a few excerpts from Kay’s story, if you’d like to download and read her full story please click here.
Getting the diagnosis
 Having suffered with migraines for years and trying a number of different medications my GP referred me to the neurology department at the hospital, after waiting 6 months I finally had an appointment on 8th February this year where I discussed my symptoms and requested an MRI scan. I had the MRI scan 4 weeks later on 11th March.
Having suffered with migraines for years and trying a number of different medications my GP referred me to the neurology department at the hospital, after waiting 6 months I finally had an appointment on 8th February this year where I discussed my symptoms and requested an MRI scan. I had the MRI scan 4 weeks later on 11th March.
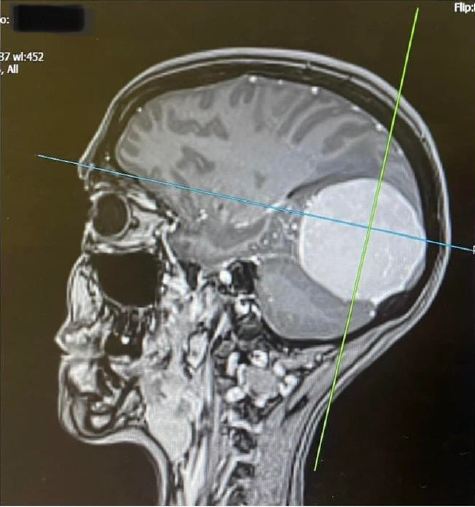
Driving home from work on 14th March, I had a call from the hospital asking me to go in the following day to discuss the results and that I should probably bring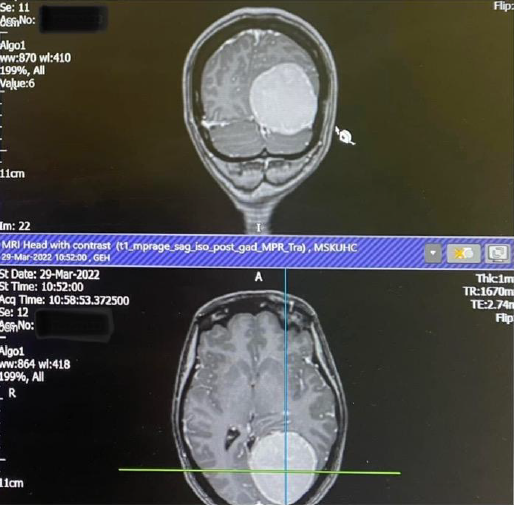 someone with me. I knew instantly that it didn’t sound good but tried to stay positive. The next day the neurologist told me that the scan showed that I had a large Meningioma in my occipital lobe, these tumours are usually benign and slow growing, but as mine was already quite big I would need surgery to remove it as there really was no other option. What a shock! I don’t know what I expected to hear but it wasn’t that. I was told the surgery would probably be within weeks, it was a lot to take in. I had bloods done there and then in preparation and cried all the way home.
someone with me. I knew instantly that it didn’t sound good but tried to stay positive. The next day the neurologist told me that the scan showed that I had a large Meningioma in my occipital lobe, these tumours are usually benign and slow growing, but as mine was already quite big I would need surgery to remove it as there really was no other option. What a shock! I don’t know what I expected to hear but it wasn’t that. I was told the surgery would probably be within weeks, it was a lot to take in. I had bloods done there and then in preparation and cried all the way home.
Waiting for surgery
I had an appointment with the neurosurgeon at UHCW on 14th April, he showed me the MRI scan and I was shocked at how big the tumour was (5.9cm), we discussed the surgery and the risks and he basically told me it had to come out and he would prefer it to be sooner rather than later so he added me to the list and I just had to wait for a date.
The not knowing drove me mad, when would the surgery be? Would I be ok? What if I wasn’t? Should I have it? During this time I continued to work and I hadn’t told many people my situation, partly because I just wanted things to be as normal as possible and partly because I’m no good with sympathy and didn’t want people treating me differently, I think there was also a part of me that thought if I didn’t talk about it then it wasn’t happening, although it was constantly on my mind and I thought about it from the second I woke up until the second I went to sleep and every second in between!
Undergoing surgery
 10th May, the day before my op was one of the worst days in my life so far, thinking that I might not ever see anyone again, or things might not be the same after surgery, just trying to get through the day the best I could but I don’t think I have ever been so terrified in my life. Visiting time came and saying bye was so hard, I cried a lot and for a long while afterwards.
10th May, the day before my op was one of the worst days in my life so far, thinking that I might not ever see anyone again, or things might not be the same after surgery, just trying to get through the day the best I could but I don’t think I have ever been so terrified in my life. Visiting time came and saying bye was so hard, I cried a lot and for a long while afterwards.
Surprisingly I slept quite well, woke up had a shower, put on my gown and I FaceTimed Lee and the kids before they went to school and then boom I was ready, let’s do it!
I was taken down at 8.52am, I remember the time as I sent my last text to Lee. I woke up in Critical Care at 7.15pm, although I was a bit out of it I actually felt ok, the op was a success and they  believe they had removed all of the tumour, my blood pressure was a little high and fluid was being drained from my brain but they were hoping to move me to a ward the next day. I had an ok night, not much sleep, a little uncomfortable, very thirsty, wires and cannulas sticking out of me everywhere but all was good…I was alive!
believe they had removed all of the tumour, my blood pressure was a little high and fluid was being drained from my brain but they were hoping to move me to a ward the next day. I had an ok night, not much sleep, a little uncomfortable, very thirsty, wires and cannulas sticking out of me everywhere but all was good…I was alive!
I spoke to Lee on the phone the next morning and he and my mum were coming to visit at 11am, I was counting down the hours, couldn’t wait to see them. I was sitting up, I’d even had breakfast and a cup of tea by the time they got there and they couldn’t believe how well I looked. I did it, I actually did it! I was moved to the ward later that day. The drain was removed and I felt quite well although very tired and I kept hallucinating when I closed my eyes which worried me slightly, although when I mentioned this to the doctor he said it was quite common after surgery of this kind and it could also be a side effect of the medication! Phew! (This lasted a few days) I was assessed on my walking ability, vision and movement
on 15th May and spoke to the consultant who said I should be able to go home the following day!
16th May, 5 days after a 7 hour craniotomy and 18 days in hospital I was discharged, I’ve never felt so happy to be going home where I belong and to see my family and friends! What a journey!
Life after surgery
When I first arrived home I spent almost every day in bed and slept so much bit woke up at silly times during the night for hours on end but it did get easier and after a couple of weeks I was making it downstairs for a few hours at a time, I had my staples removed 11 days after surgery and the wound looked to be healing well.
and after a couple of weeks I was making it downstairs for a few hours at a time, I had my staples removed 11 days after surgery and the wound looked to be healing well.
On 18th July, 9 and a half weeks after my surgery I returned to work, this was only on a part time basis for 4 days but was a step in the right direction and something I wanted to do (I work in a school so it was coming up to Summer holidays).
A week after we jetted off on our hols, although very hot and very tiring the holiday was just what we needed and even though I have non stop slept since we got back we had the best time with some of our best friends and the flight was fine.
I’m still suffering with tiredness and fatigue and other people who have been through the same have said this can last months and maybe even years so I guess this could just be a new way of life that I have to get used to. I’m taking anti convulsant medication which I will continue with for at least a year to prevent seizures which up to now I have not suffered with pre or post op and I’m still waiting to hear back from DVLA regarding my driving license but my consultant did say I couldn’t drive for 12 months so I’m following that advice until I hear differently which you don’t realise how much this impacts you until it happens, luckily I have a very good friend who has offered to take me to work and takes me out when the 4 walls get too much! Thankfully there have been no migraines since April and I hope it stays that way.
What I want the world to know
One thing I will say is just because I’m smiling doesn’t always mean I’m ok, some days are harder than others but I’m still here to tell my story and I couldn’t have done it without my amazing family and friends.
Life goes on….
Don’t sweat the small stuff!