Hi! My name is Katie, I am 25 years old, I am currently living in the lovely Kent countryside just outside of Southeast London. I work in a local secondary school after graduating from my Bachelor’s Degree in Biomedical Science last summer. I am part of an amazing family with the most supportive and caring parents and grandparents, I am one of 6 siblings, and I am an aunt to four of the funniest, kindest children you’d ever meet. I am also blessed to have been with my partner Tony for 8 years and we enjoy exploring different places, trying different cuisines, and watching films together – we have done even more of this since my diagnosis.
Bachelor’s Degree in Biomedical Science last summer. I am part of an amazing family with the most supportive and caring parents and grandparents, I am one of 6 siblings, and I am an aunt to four of the funniest, kindest children you’d ever meet. I am also blessed to have been with my partner Tony for 8 years and we enjoy exploring different places, trying different cuisines, and watching films together – we have done even more of this since my diagnosis.
I wanted to tell my story to firstly highlight my condition as we are roughly 3 in a million and are often underrepresented. And secondly to show any newly diagnosed colloid cyst patients that there are people out there who will support us – and those people are the brainstrust team.
Receiving a diagnosis during the Covid-19 pandemic
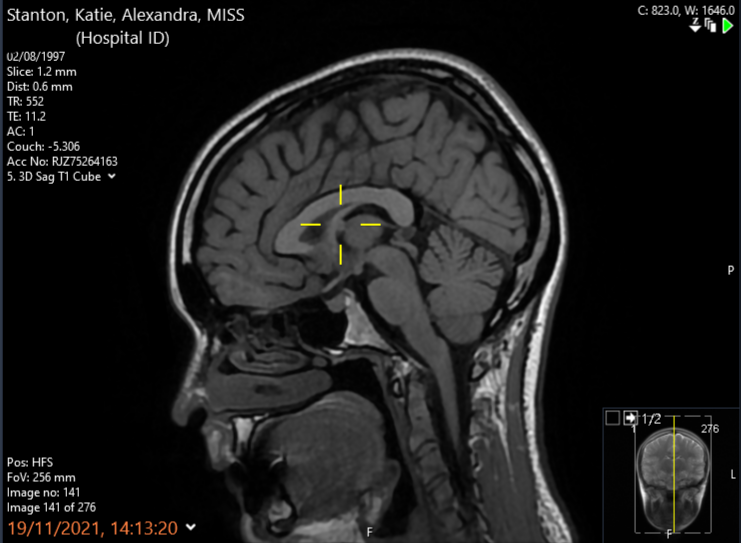 In August 2021 I received my diagnosis; an intraventricular tumour called a colloid cyst, located within the third ventricle of the brain – which is right in the middle. The cyst was found after a long string of headaches lead me to urgent care with visual disturbances, resulting in a referral for a CT scan. The scan revealed the cyst at an early stage, and thankfully no sign of hydrocephalus (cerebrospinal fluid building up around the brain due to the cyst blocking the flow) meaning that I was able to be put on Watch & Wait with yearly monitoring scans every November.
In August 2021 I received my diagnosis; an intraventricular tumour called a colloid cyst, located within the third ventricle of the brain – which is right in the middle. The cyst was found after a long string of headaches lead me to urgent care with visual disturbances, resulting in a referral for a CT scan. The scan revealed the cyst at an early stage, and thankfully no sign of hydrocephalus (cerebrospinal fluid building up around the brain due to the cyst blocking the flow) meaning that I was able to be put on Watch & Wait with yearly monitoring scans every November.
As this was during the Covid-19 pandemic, the diagnosis was delivered over the phone by my GP which was incredibly hard to deal with. The best way to describe my feelings at the time was a mixture of fear paired with an overwhelming sense of confusion. As how could this be happening to me? I had just finished my degree that I had worked hard for, I was starting a new job that I was excited for at the end of the week, and I had just turned 24 years of age a few weeks prior. It felt like such a cruel twist of fate for this to happen as my life was just coming together how I wanted.
Coming to terms with my diagnosis
After my diagnosis, my first thought was to join a support group to gain first hand information from other patients suffering from the same illness as myself. However, I quickly realised that this was not the right decision (for me) as I became overwhelmed and scared after reading some stories documenting patients experiences. I quickly left the group and prematurely resigned myself to the fact that my life would never be the same.
However, after taking some time to process what was happening, I was not ready to give up and decided to read as many scientific journals as I could get my hands on. Having just graduated with a Biomedical Science degree, this was a comfortable way for me to digest information without confronting the emotional side of the illness – as I just simply wasn’t ready or able to do that yet. A few months passed, I learned as much as I possibly could about the condition and felt comfortable with what to expect moving forward. I also felt able to re-join a support group on social media as they can be an amazing space for support and information sharing, but I must admit I check them less and less with each passing month as my life returns to normal and my diagnosis becomes part of my life, not my whole life.
Finding brainstrust
I first discovered brainstrust by seeking a charity that was working to support people with my condition, in the hopes of doing some fundraising for them in the future as I have done with multiple other charities over the years. I then began to read the brainstrust website and stumbled across a page that outlined different types of brain tumours and there my condition was in the list. Due to the rarity of my condition there is a huge lack of information surrounding it so I was surprised but also extremely pleased to be represented. Upon seeing this, I applied for a brainbox as I hoped that the resources inside would help me to cope with my diagnosis and manage any future outcomes.
brainstrust has supported me greatly. After applying for my brainbox, Molly reached out to me to introduce herself as the support specialist that covers my area and has since been a big support, answering any of my questions and helping me to fulfil my desire of raising awareness for my condition by putting me in touch with brainstrust’s own colloid cysts focus group that was focused on creating resources for colloid cyst patients both pre- and post-surgery. The focus group helped me to feel not so alone in my condition as over Zoom I could finally see some faces that were going through the same experience as me. The group also gave a positive spin to my diagnosis as helping to create resources for other patients gives a sense of purpose to the pain (both physical and emotional) that we go through.
 What I want the world to know about life with a brain tumour
What I want the world to know about life with a brain tumour
Getting a brain tumour diagnosis does change you and your outlook on life, so don’t try to be the same person as you were before but embrace your new world and the challenges that face you. Also take some time to think about what you actually want from your life, as brain tumour or not we are all only here for a short time, and we need to make the most of it. Since my diagnosis I don’t worry about things anymore and I am always up for something new or a challenge, as why not! For example, I have always been scared of open water, but I have challenged this and have been on open boat tours to see the Maunsell Forts and sea lions off the coast of Whistable. A great experience that I would never have attempted before my diagnosis.
My advice for others going through a similar situation
There is no right or wrong way to deal with a diagnosis, but my advice would be to take some time to yourself before diving into the world of other people’s experiences until your initial emotions have settled down and you are ready to deal with that side of things. Spend time initially understanding what is going on for you and how you would like to deal with your own journey before seeking stories of other people’s progress – as all our journeys will be different and it is best not to scare yourself with ‘what ifs’ and comparisons to other patients.