 With 12,000 people diagnosed with a brain tumour every year, and with March being UK Brain Tumour Awareness Month, there has never been a more important time to recognise the work of the teams that have helped patients through their brain tumour journey
With 12,000 people diagnosed with a brain tumour every year, and with March being UK Brain Tumour Awareness Month, there has never been a more important time to recognise the work of the teams that have helped patients through their brain tumour journey
-
More on this announcement
-
Has your hospital been successful?
-
What does it mean if my hospital isn’t one of the nine centres?
-
What do the hospitals say?
-
What happens next?
-
About the Tessa Jowell Brain Cancer Mission
More on this announcement
- The newly introduced ‘Tessa Jowell Centre of Excellence status’ recognises the delivery of outstanding care and treatment by NHS staff in their efforts to provide above excellent patient care through a difficult time
- Three years ago, Baroness Tessa Jowell gave her powerful speech in the House of Lords recognising the need to improve brain tumour treatment, care and survival for all patients
- Brain tumours are often found at later stages; only 12% of adults survive for five years after diagnosis highlighting the need for further innovation in brain tumour care
- The mission is delighted to be embarking on the pathway to excellence with the 20 applicant centres, nine of whom have already achieved centre of excellence status in the first round.
Nine NHS hospital brain tumour centres across the UK have been recognised as a Tessa Jowell Centre of Excellence following the first round of rigorous expert-led assessments by the Tessa Jowell Brain Cancer Mission.
With more than 12,000 people diagnosed every year with a primary brain tumour in the UK, the award has been introduced to recognise hospitals for their excellence in patient care. It represents a step change in the neuro-oncology landscape across the UK. Centres were measured on a range of criteria including excellent clinical practice and training opportunities; emphasis on patient quality of life; providing clinical trials and offering a high standard of research opportunities. Led by a committee of experts in the field and virtual site visits, the assessments were backed up by patients, validated by those who are living with a brain tumour diagnosis.
At least 88,000 British people are currently living with a brain tumour and over 5,000 people a year will lose their lives to it. The “Excellence” status provides reassurance about the availability of excellent care within the NHS and positive recognition for its staff who, despite the challenges of the Covid-19 pandemic, continue to go above and beyond for their patients. As a result, centres are increasingly adapting to the challenges of Covid-19 and are now offering virtual clinics for their patients.
Founded to design a new national strategy for brain tumours, the Tessa Jowell Brain Cancer Mission is committed to helping as many hospitals as possible achieve “Excellence” status in the future. To achieve this, the mission is launching the Tessa Jowell Academy, a national platform allowing hospitals to share best-practice to improve their services, as well as one-year fellowships for doctors to further specialise in brain tumours. It is hoped that with the support of the Academy more centres will qualify for excellence status in the future, extending the reassurance of excellent NHS care more broadly and ensuring no patient is left behind.
 Jess Mills, Co-Founder of the Tessa Jowell Brain Cancer Mission and Tessa’s daughter, said: “Mum’s mission throughout 50 years of her political life was to tackle systemic inequality. So, it was tragic whilst fitting, that her final campaign was a call to arms to create universal equality in access to excellence in cancer care throughout the NHS. It is with immeasurable pride that just 3 years later, the Tessa Jowell Brain Cancer Mission has begun the real-world translation of that vision into reality.
Jess Mills, Co-Founder of the Tessa Jowell Brain Cancer Mission and Tessa’s daughter, said: “Mum’s mission throughout 50 years of her political life was to tackle systemic inequality. So, it was tragic whilst fitting, that her final campaign was a call to arms to create universal equality in access to excellence in cancer care throughout the NHS. It is with immeasurable pride that just 3 years later, the Tessa Jowell Brain Cancer Mission has begun the real-world translation of that vision into reality.
“We are thrilled to have awarded nine centres for their excellent ongoing work for patients and commitment to support other centres in reaching the same level of Excellence. Shockingly, the UK still has one of the worst cancer survival rates in Europe, but in time, the Tessa Jowell Centres will make the UK a global leader in the treatment and care of brain tumour patients. We have a long way to go until the cutting edge of science is delivered to every patient, but this is a huge and transformational first step.”
Which hospitals have been successful?
Tessa Jowell Centres of Excellence:
- University Hospitals Birmingham NHS Foundation Trust
- Edinburgh Centre for Neuro-oncology
- King’s Health Partners / King’s College Hospital & Guy’s and St Thomas’s Hospitals
- Leeds Teaching Hospitals NHS Trust
- Salford Royal Foundation Trust and The Christie
- Newcastle upon Tyne Hospitals NHS Foundation Trust
- Nottingham University Hospitals
- St George’s University Hospital, Royal Marsden Hospital and Royal Surrey County Hospital
- University College Hospital London NHS Foundation Trust
Over £700M is spent on cancer research in the UK every year, yet less than 2% of that is dedicated to brain tumours. The Mission, which will be supported by the All-Parliamentary Group on Brain Tumours chaired by Derek Thomas MP, is calling upon further support for NHS centres to enable more of them to achieve “Excellence” status in the future.
 Professor Richard Gilbertson, Chair of the Mission, highlights: “When we put out a call to apply, we received an overwhelming and enthusiastic response from the community. There was a real sense of pride from NHS staff about the service they have been providing and how they strive to provide the very best care for patients, even in the midst of a pandemic.
Professor Richard Gilbertson, Chair of the Mission, highlights: “When we put out a call to apply, we received an overwhelming and enthusiastic response from the community. There was a real sense of pride from NHS staff about the service they have been providing and how they strive to provide the very best care for patients, even in the midst of a pandemic.
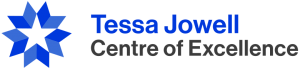
All of these centres excelled during their rigorous assessments in 5 key areas. They deliver excellent treatment; have an emphasis on patient quality of life; offer opportunities to engage with brain tumour research and trials; provide good training and development opportunities for staff; and they are site for excellence and innovation in brain tumour research.
What does it mean if my hospital isn’t one of the nine centres?
First of all, not every hospital was ready to apply with many deciding to defer their application because of the pressures of COVID-19 on care. For many, this has taken precedent.
Professor Richard Gilbertson also says:
All applying hospitals were working to provide best care and we will be supporting those not yet ready for Centre of Excellence status to enact best practice across all areas. We will use the evidence collected from the applications forms to make a strong case to further equip these centres.”
Will Jones, Chief Executive at brainstrust and TJBCM Joint Strategy Board member adds:
We should all be excited about the change that this represents, no matter which hospital is looking after us. The challenge now is manifold as we strive together as a community, for the community, to move every UK centre that treats people with a brain tumour from good to great.
The hope is that every centre can become a centre of excellence. In the meantime, care across the UK at all hospitals is safe and it is good. If you have any questions or concerns then speak to your clinical team, or call us at brainstrust and you will get the help you need.
Today, right now, you can already see if your hospital is delivering a standard of care to NICE guidance, and also get help with what to expect on your journey by reading the brainstrust patient guides. More on these here: www.brainstrust.org.uk/patient-guides/
The NICE guidance in itself sets a bar for excellence.
What do the hospitals say?
Cally Palmer, NHS England national cancer director, sets the scene “This award is a fitting tribute to Tessa Jowell and her dedication to excellence in cancer care, as well as to all the NHS staff who have worked tirelessly throughout the pandemic to continue to provide life-saving cancer services, and it is great to see NHS hospitals across the country being recognised as centres of excellence.
“NHS services are open and ready to help those who need cancer care, and I encourage anyone who is experiencing any worrying symptoms to contact their GP immediately to improve chances of a successful recovery.”
Birmingham Queen Elizabeth Hospital
We are delighted that our model of patient-centred, consultant-led, research-orientated care for brain cancer patients has been recognised in this way. This award is a tribute to the whole multidisciplinary team who put patients at the centre of everything they do and take real pride in delivering best practice for everyone. Prof. Colin Watts – Chair Birmingham Brain Cancer Program and honorary consultant neurosurgeon
Leeds Teaching Hospitals Trust
We are immensely proud of the excellent care delivered by the whole neuro oncology team in Leeds and very pleased to be able to contribute to a national effort to improve the experience of all brain tumour patients through designation as a Tessa Jowell Centre of Excellence ‘ Prof Susan Short – Professor of Clinical Oncology and Neuro-Oncology
King’s College Hospital and Guy’s and St Thomas’
“Designation as a Tessa Jowell Centre of Excellence is an immense honour and privilege for my team and I. It reassures and reinforces the team to continue on their chosen path to provide excellent care; it builds confidence in the service for our patients; and it provides us with the legitimacy to fight for resources we believe are needed even harder to do even better for our patients; after all they deserve nothing less.”
Prof Keyoumars Ashkan, Professor of Neurosurgery and Clinical Lead for Neuro-Oncology)
Newcastle Hospitals
“This fantastic honour will mean so much to the patients of the North East and Cumbria knowing that they are receiving care in a centre of excellence. The wider Newcastle/North East neuro-oncology team are delighted that there is recognition of their efforts to provide such a high standard of care.
“It is the Geordie “shy bairns get nowt” tenacity of so many members of the team that has resulted in the holistic, integrated multi-disciplinary care pathway for patients and specialist interventions such as bevacizumab for symptomatic radiotherapy effects.
“We look forward to supporting the Tessa Jowell Brain Cancer Mission in its aim to promote excellence in care for brain tumour patients and assisting the Tessa Jowell Academy in disseminating evidence of great practice. No one unit gets everything right all the time so we know there is a lot we can learn and hopefully help other units too.”
“To be designated by the Tessa Jowell Brain Cancer Mission is a great honour for the team,” adds Dr Joanne Lewis, Consultant Clinical Oncologist at the Freeman Hospital’s Northern Centre for Cancer Care.
“The recognition of our “human centred culture of kindness and compassion” was the highest compliment we could have wished for. I am excited by the opportunities we have to push forward change for brain tumour patients, we are also keen to adopt best practise and learn from the Tessa Jowell Academy. This award has made us even more determined to give our patients the best possible care.”
Damian Holliman, Consultant Neurosurgeon and Neuro-oncology MDT Lead
What happens next?
There is a road map here for excellence to become the norm. This is an important moment for the brain tumour community no matter who or where you are in the UK. We should first congratulate these first 9 centres and with the community’s continued support in not too many years to come, the gold standard should become the normal standard – people with a brain tumour can be confident that they will be getting the best possible care so that they can live their best possible lives in the face of their diagnosis.
The biggest challenge that faces the Mission now is to make sure excellence is shared so that others can attain Centre of Excellence Status, and to ensure that support is in place so that the rigorous process of accreditation and review can be sustained and scaled. The mission is a ‘convening body’ that receives its funding from the partner organisations, so your ongoing support of brain tumour charities, like brainstrust will help this to happen.
About the Tessa Jowell Brain Cancer Mission
 The Tessa Jowell Brain Cancer Mission is supported by the Department of Health and Social Care and brings together leading clinicians and academics, Brain Tumour Research, Cancer Research UK, The Brain Tumour Charity, brainstrust, Brain Tumour Support, The Minderoo Foundation, The Tessa Jowell Foundation, Act for Cancer and the National Cancer Research Institute, amongst others.
The Tessa Jowell Brain Cancer Mission is supported by the Department of Health and Social Care and brings together leading clinicians and academics, Brain Tumour Research, Cancer Research UK, The Brain Tumour Charity, brainstrust, Brain Tumour Support, The Minderoo Foundation, The Tessa Jowell Foundation, Act for Cancer and the National Cancer Research Institute, amongst others.
In her famous last speech in the House of Lords, Baroness Tessa Jowell appealed for society’s big problems to not be put into the “too difficult box”. The Tessa Jowell Brain Cancer Mission was later set up to deliver the MP’s defining public health strategies and design innovative solutions to transform brain tumour treatment, research and survival to ensure all patients across the UK receive the best possible care, regardless of where they live. It serves as a convening body for these organisations, enabling them to work together to make a tangible change in brain tumour treatment and research. TJBCM is neither a charity, fundraising nor grant-awarding body.
Over the next five years the TJBCM is focusing on six strategic objectives, organised through individual Strategic Programmes. The mission is working on initiatives in the areas of patients, clinical trials, training for physicians, research, emerging data and technology and the Tessa Jowell Centre Designation. The Centre designation programme was chaired by Emerita Professor Kate Bushby from Newcastle University, whose husband Jimmy Steele died with a glioblastoma in 2017.
In line with Tessa’s aspiration of “I hope that cancer patients like me, can live well with cancer, not just be dying of it,” the reviewers paid special attention to neuro centre’s patient quality of life care and looked for a culture of kindness and respect. The Tessa Jowell Centres of Excellence will form a world-class network of brain tumour treatment and research centres, providing patients with access to the very best treatment and research opportunities.










