Information about meningiomas
On this page, you will find information about meningiomas, including the different types, grading and possible symptoms.
For more information about our meningioma support network visit our meningioma webpages here.
Meningiomas are a type of brain tumour. A meningioma is a tumour that starts in the meninges. The meninges are layers of tissue (membranes) that cover and protect the brain and spinal cord. There are three layers:
- The dura mater. This layer surrounds and supports the large channels that carry blood from the brain toward the heart.
- The arachnoid. This middle layer helps protect the brain and spinal cord from sudden impact.
- The pia mater. This layer is next to the brain and follows its contours. It acts as a barrier and aids in the production of cerebrospinal fluid.
This two-minute video explains the meninges and the layers.
Most meningiomas are slow-growing tumours, although some can grow faster. Although the majority of meningiomas are non-malignant, these tumours can grow slowly until they are very large, if left undiscovered. In some locations, they can be severely disabling and life-threatening. Other forms of meningiomas may be more aggressive. Most patients develop a single meningioma; however, some patients may develop several tumours growing simultaneously in other locations in the brain.
We don’t know why these tumours start, although there are predisposing factors associated with meningiomas. These include exposure to radiation (e.g. in the treatment of childhood cancers, such as leukaemia), prolonged use of certain hormones (e.g. in gender-reassignment treatment) and some genetic disorders (e.g. neurofibromatosis). We know that non-malignant meningiomas are also more common in women than in men, and they may show increased growth during pregnancy.
A word about benign meningiomas. At brainstrust, we don’t use the word benign. We call these tumours non-malignant. About 80%–90% of meningiomas are non-malignant. It is hard calling something benign when these tumours can be life-changing, disabling and come with a high symptom burden. Calling a meningioma benign can devalue the impact that it has on someone’s life.
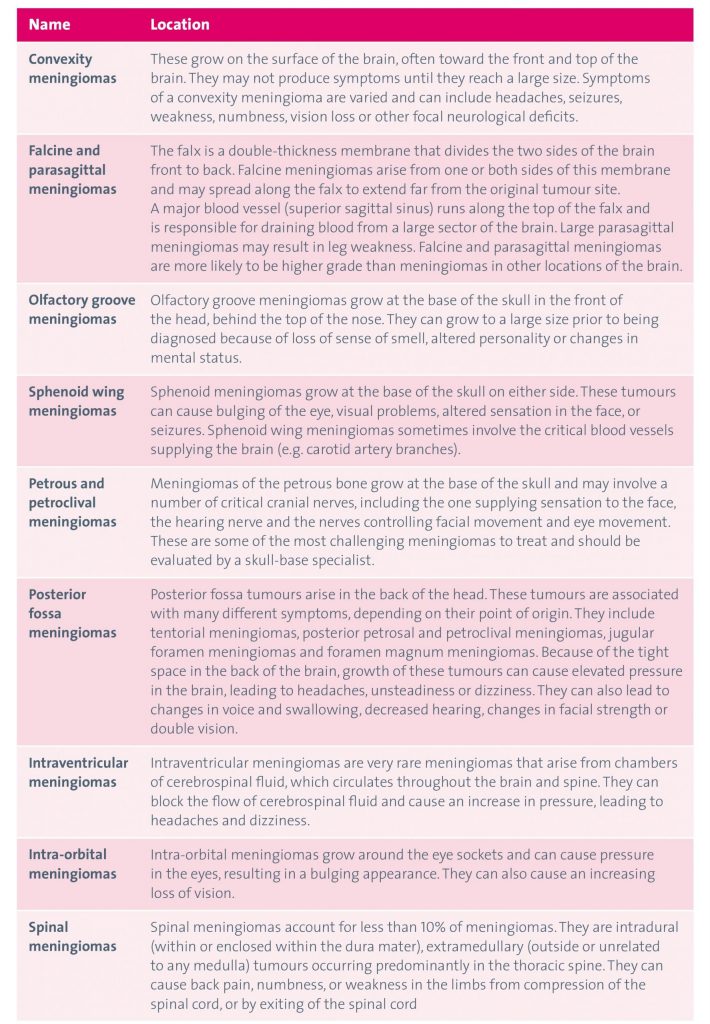
The World Health Organization (WHO) classification of brain tumours is the most widely used tool in grading brain tumour types. The WHO classification scheme recognises variations of meningiomas according to their cell type as seen under a microscope. These variations are called meningioma subtypes – the technical term for these variations is histological subtypes. These histological subtypes are organised into three grades, which generally reflect the rate of growth and likelihood of recurrence.
Table of meningioma subtypes
This is where it gets a little complicated. Meningiomas are graded I to III. Grading is based on histopathology – the study of the disease and the cells and tissues. So in this instance, histopathology can only be achieved by doing a biopsy or removing the meningioma, and that would then be sent for analysis.
Grades of meningiomas
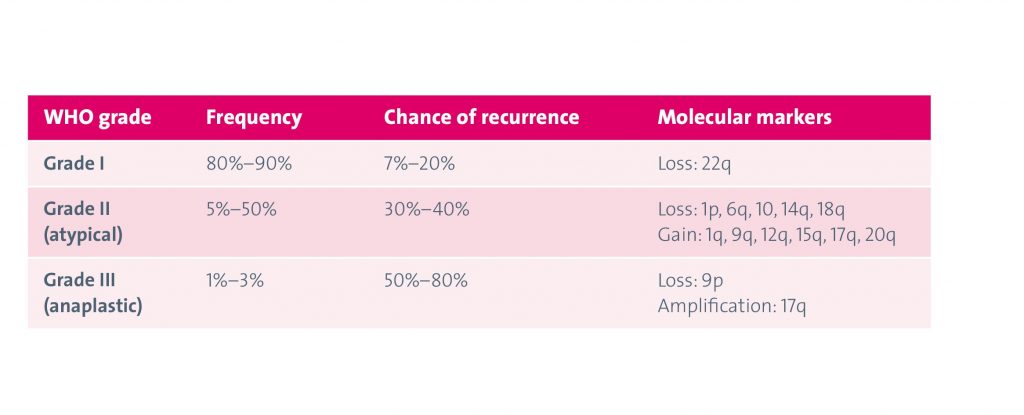
Meningiomas are typically slow-growing tumours, with the most common classification of meningioma being grade I. This means that most symptoms will occur gradually, if at all.
Not all meningiomas cause symptoms, but symptoms may be caused by the tumour pressing on other parts of the brain as it grows, or a build-up of pressure. This means that symptoms will vary according to the size, location and growth rate of the tumour.
Possible symptoms include:
- new, persistent headaches
- nausea or vomiting
- behaviour and personality change
- confusion
- drowsiness
- weakness in an arm or leg
- balance issues
- seizures (fits)
- sight problems.
If you are concerned about any symptoms, always seek medical advice.








