Follow-up support
Some time may have passed following your diagnosis, and while you no longer find yourself in the shock of new, you may still find yourself needing a little extra support to help you live the life you want. Sometimes, knowing what you can expect in terms of follow-up care can help you to feel better prepared and more in control.
What is follow-up care?
Follow-up care is the transition from your initial diagnosis and treatment plan to living with your diagnosis for the longer term, when you may not have such close contact with your clinical team. It can feel a little like you have been cast adrift. It’s okay to feel like this. Your treatment plan may have included surgery, radiotherapy or chemotherapy, or you could be on active surveillance. Whatever treatment you have, it is important to know what is next.
The optimum standard of care according to the NICE Improving Outcomes Guidance for the follow-up phase of care includes:
- routine imaging
- regular clinical reviews to assess changes in your physical, psychological and cognitive well-being
- ready access to assessment and rehabilitation services for problems such as epilepsy, headaches, and speech or visual problems
- ready access to specialist neuropsychology and neuropsychiatry services
- immediate access to specialist equipment that would assist rehabilitation as necessary
- clear information on who to contact and how if you are concerned about your condition
- follow-up as close to home as possible.
The above is the minimum level of care that you should expect at this stage. However, sometimes, for a variety of reasons, our healthcare service may not be able to meet these standards.
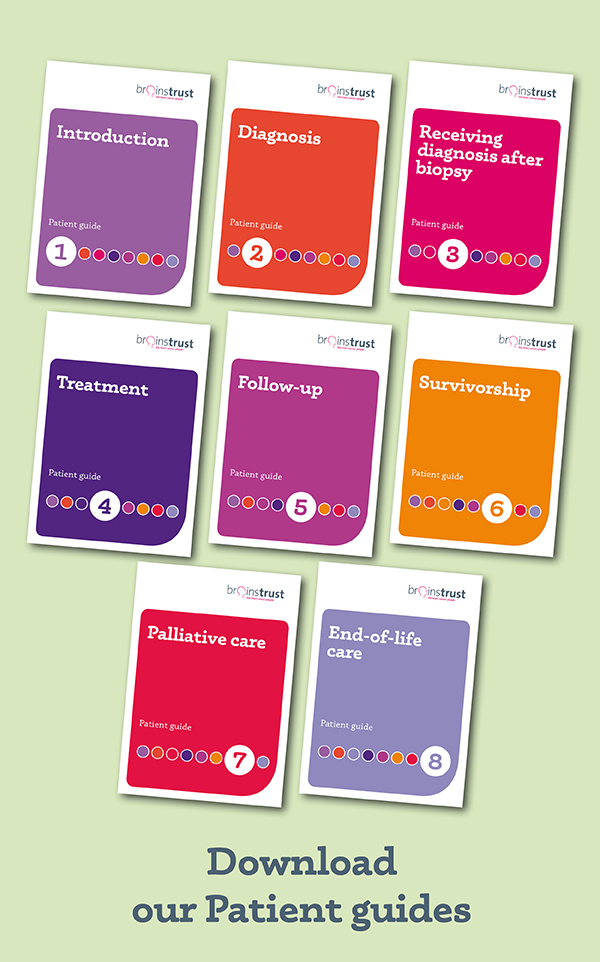
These standards of care have been taken from our ‘Follow-up’ patient guide. Our patient guides are a brilliant resource designed to help guide you through the patient pathway and know what your options are.
How can I access the support I need?
Hospitals often have different services that they are able to provide, and different means of being able to provide them. For things such as routine imaging and clinical reviews, these will be organised by your clinical team at intervals agreed by them, and hopefully in discussion with you, based on your diagnosis and condition. For some of the other services detailed above, these may include referrals to other departments or services.
Here are some tips to ensure you have clarity on what support you can get:
Ask questions. This may sound simple enough, but often in a medical appointment, you are there for a specific reason, such as finding out the result of your surgery or latest treatment, and it can be difficult to think of what questions to ask about follow-up care. Feel prepared by sitting down for a few minutes the day before your appointment and writing down the questions you want to ask.
There are some great suggestions in our patient guide
Keep a record of your symptoms and things that you feel you need support with. Our ‘Who’s who in your clinical team’ guide can help to give you an overview of who in your team might be able to help.
Access ‘Who’s who in your clinical team’ guide
Speak to brainstrust. While we won’t be able to give you medical advice, we can help to elicit the questions that you want to ask. We can also signpost you to who can help and provide you with information and resources so that you feel more in control and involved in your clinical care.
How can brainstrust help?
- We can use our coaching models to help you focus on what matters to you the most at the moment and achieve clarity.
- We can signpost you to the right information and resources to help you make informed choices and decisions, and point you in the right direction.
- We run webinars and workshops on topics that are important to you when you are living with a brain tumour diagnosis.