 NHS Patient Centred Communication
NHS Patient Centred Communication
The NHS has produced guidance[1] that outlines key principles to help clinicans deliver personalised, patient (we’d prefer person) centred communication to you if you are waiting for care.
We’ll share the key principles here, so people with a brain tumour:
- Have a better understanding of whats at play, if treatment is delayed,
- Can engage constructively with their clinical team to ensure the best outcomes.
COVID-19 has impacted in so many ways. We know people are facing delays in scanning and surgery, and changes to treatment plans – especially the members of our community with low grade and non-malignant tumours.
This uncertainty is hard to live with, but has to be balanced with the risk versus benefit. For example, the risk of having surgery and then not having access to the necessary care afterwards due to lack of beds or staff shortages, would outweigh the benefit.
How are decisions made, and how can you play an active role in decision making?
Making these decisions is incredibly difficult for all involved – patients, caregivers and healthcare professionals (HCPs) alike. Communicating when we are stressed, even without the added pressures of COVID-19, is a tough ask. HCPs have to define how much information a patient wants, nurture hope when the future looks bleak, and manage the expectations of patients and caregivers when their wants and needs differ. Of course, for people living with a brain tumour, the uncertainty, fear and disappointment are incredibly hard to manage.
The key principles outlined by the NHS to help clinicians deliver personalised, patient centred communication to you if you are waiting for care are explained below.
At any point when you’re reading these, do get in touch with us. Call your support specialist, email us or call our helpline on 01983 292 405.
Personalised communication
This means that you should be told about the next steps of your care pathway and the likely timescales. This should mean that you can discuss the risks and benefits of any delay. Talk about your worries and your fears – explain how the delay makes you feel and ask what support is available to you.
Clear language
Language should be easy to understand, clear and accessible. If any technical terms are used always ask for an explanation.
Shared decision making
Making decisions together that are right for the patient is called shared decision making. You have a right to be involved in discussions and make informed decisions about your care.
- You are the expert on you! You know what your context is, what your appetite for risk is and what your values are.
- Clinicians are the experts on what options are available.
Making shared decisions needs preparation and thought – it doesn’t just happen. It is a collaborative process that involves you and your HCP working together to reach a joint decision about your care. It could be care that you need straightaway, or care for further down the line (e.g. advance care planning).
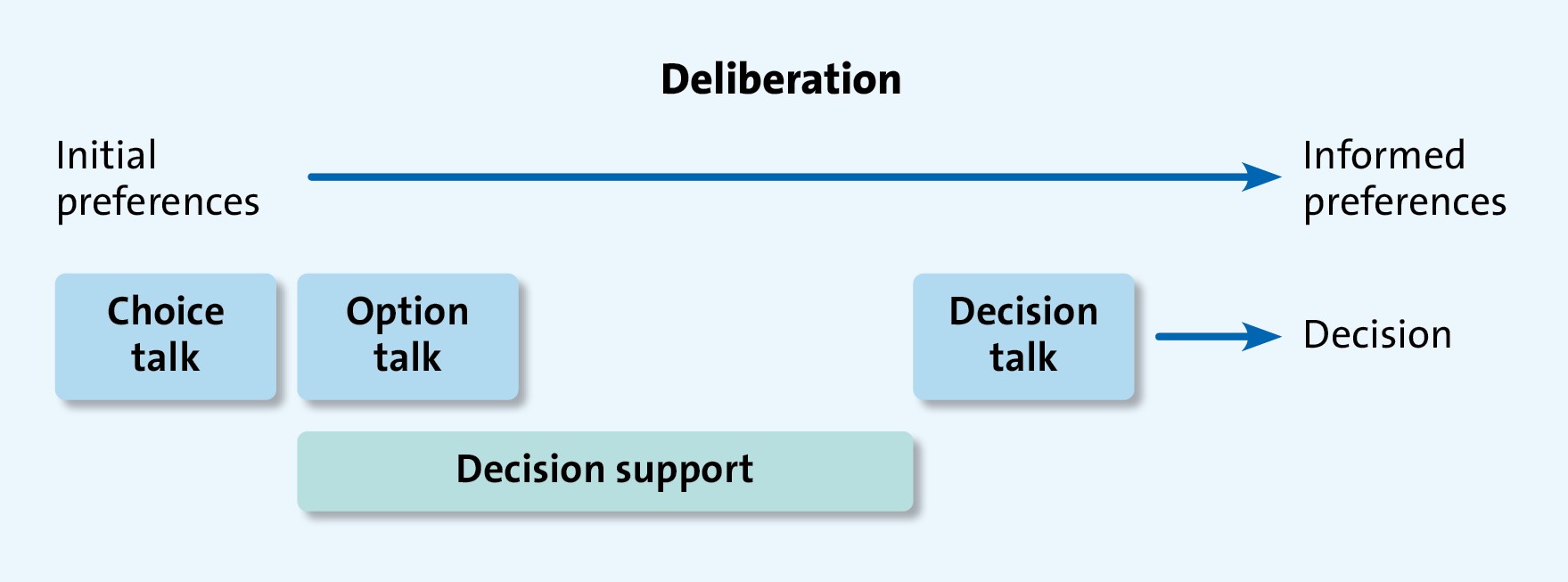
Three-talk model[2]
The most accessible and easily embraced model is the three-talk model. This is a practical model of how to do shared decision making that is based on following choice, option and decision talk stages during the consultation.
The model has three steps:
- Choice. The patient asks ‘What are my options?’
- Options. Often described by integrating risks v. benefits. The patient asks ‘what are the pros and cons of each option for me?’
- Decision. Helping people explore their preferences and make decisions. The patient asks ‘What do I need to help me make a decision that is right for me?’
 Patient safety
Patient safety
The NHS is open for those that need it. Hospitals are doing all they can to reduce the risk of catching COVID-19. You should feel able to discuss the balance between the need for treatment versus the risk of coming into hospital with your clinical team.
If you’re being asked to attend a hospital appointment, all steps to keep you safe from COVID-19 have been taken. Some scanners are being kept ‘clean’, for example. This means no patient who has tested positive for COVID-19 will use that scanner. Separate entrances and pathways have been set up for COVID-19 free patients.
Managing appointments, delays and cancellations
Clinicians are asked to provide a clear message with compassion if your care is being delayed. They should be clear about next steps, and honest if they don’t know when things will happen.
Contact points
You should be given a point of contact – someone you can call to get information. You should be able to leave a message out of hours and have an email contact too.
Some hospitals have set up a single point of contact (SPOC) to make things easier.
Interim information
If your treatment plan is changed, then alternative options should be discussed with you. If your condition gets worse, you should know who to contact.
Cancellation policy
You should know how to cancel your care if you want to. Likewise, if your clinician cancels your care this should be done with compassion, and in line with the Trust’s policy.
Communication strategy
Every Trust is different. There should be local updates about the impact of COVID-19 in your area, and timeframes for when care is likely to return to pre-COVID-19 levels.
We all have a role to play to make communication a positive experience. If you have any concerns about your care please talk to your clinical team – the NHS is very much open.
Get in touch today to find out more about how we can help you engage with your clinical care.
[1] https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2021/01/C0855_i_Good-communication-with-patients-21-January-2021.pdf [accessed February 25, 2021]
[2] Elwyn Glyn, Durand Marie Anne, Song Julia, Aarts Johanna, Barr Paul J, Berger Zackary et al. A three-talk model for shared decision making: multistage consultation process BMJ 2017; 359 :j4891










