As face coverings become mandatory in more circumstances across the UK, we want to help combat any anxiety they may cause you whilst keeping you safe.
Unless we are medically exempt, it is now (or soon will be) our obligation to wear a face covering in certain public places, such as on public transport and in shops. These do not need to be PPE or medical quality, just a covering of your nose and mouth to help protect you and others from the spread of Coronavirus.
We have a limited amount of brainstrust branded face coverings for the brain tumour community available to pre-order. Comfortable, affordable and reusable, they meet the government’s requirements and will help you feel safe and protected when out and about.
Feeling anxious about wearing a mask?
For many of us in the brain tumour community, wearing face coverings to keep everybody safe is a positive step. Particularly for those more at risk, or looking after people that are, any action to help stop the spread of the virus makes getting back to some sort of normality more possible.
However, we know that the idea of wearing face coverings can be scary and uncomfortable too. We know that there are some consequences of brain tumour treatment that can make wearing a mask more unpleasant – such as having a permanently dry mouth, caused by radiotherapy. If you’re a glasses wearer, masks can be difficult because they fog up! Specsavers have pulled together some tips to help you avoid this.
We also understand that for all sorts of reasons, wearing a face mask can make you feel anxious. Below, Jane, one of our Support Specialists, outlines why this might be, and offers some practical tips to support you in managing this new challenge.
Why can masks provoke anxiety, and how can we overcome this?
Is the thought of wearing a mask causing you anxiety or concern? We know that many of our community are struggling with this right now, because you’ve been telling us that you are.
Anxiety encompasses feelings of worry, nervousness, or dread that something bad is about to happen. Although unpleasant, occasional bouts of anxiety are natural and sometimes can even be considered positive: taking an evolutionary perspective we know that by signalling that something isn’t quite right, anxiety can help us to avoid danger. It can also be positive in that it can provoke us to make meaningful changes.
Anxiety can be triggered when there is uncertainty, and so if the thought of wearing a mask is concerning for you this could just be a natural response from your body about a situation that’s new or uncertain and where the outcome isn’t yet defined. Quite simply, it’s normal for some people to feel anxious at the thought of wearing a mask.
Seeing others wearing a mask can also cause anxiety. This can be especially true for people living with a brain tumour diagnosis, because the medical type mask can evoke memories of past trauma from time spent in hospital and receiving treatment, as the medical professionals may have been wearing masks. Prior negative experiences can be contextual and so it may be the case that the context of seeing others wearing masks is coded as part of the traumatic experience, and so now being surrounded by this again can cause panic. This can also be true of our own specific treatment experience, for example, being fitted for a radiotherapy mask can be traumatic.
And of course, when we’re feeling anxious, the last thing we want is to feel smothered, which is how some people feel when asked to wear a mask themselves. So what are some practical steps that we can take to try to minimise the feelings of anxiety that masks can provoke?
Wearing the mask more often
In the same way that social anxiety may be alleviated by exposure therapy (where you are gradually exposed to a feared situation or object, and learn to become less sensitive over time), you may find that wearing a mask for short periods of time in a safe space, such as at home, or in the company of a trusted companion, might help. By safely and gradually exposing yourself to the concept of wearing a mask, you may slowly overcome your fear.
Know that mask wearing is safe
Long before Covid-19, healthcare professionals and others have routinely been wearing masks as they go about their daily routines. Although much of the media hype may lead us to believe that this is a new way of being, the wearing of masks has been routine for many for some time. Reassure yourself that the wearing of masks is considered to be safe.
Re-focusing
Although perhaps more easily said than done, not focusing on the small discomforts generated by the mask wearing can help. Can you distract yourself by focusing on other things, perhaps by listening to a podcast on your walk to the shop? Also remember that mindfulness practice can help here; focusing on your breathing and observing your surroundings as well as your own thoughts can be a great help.
Grounding techniques
This is a useful tool to combat feelings of panic in the moment and can help distract you from your challenging emotions and help you to reconnect with what’s around you. We know that it is helpful to be mindful of what is around us, but in times of panic, take this a little further by deliberately utilising your senses. What can you see? Try to notice 5 distinct things, perhaps in a certain colour. What can you smell? Try to identify exactly what you can smell. What can you feel? Focus on the feeling of your feet on the ground; try walking, counting your steps as you feel your feet make contact with the ground can be helpful. Perhaps touching your clothes and noticing how they feel; is your jumper soft? All of these things, as simple as they might sound, can be very effective in helping to ground us into the reality of the present situation and distract from the unwanted challenging feelings being experienced.
Understand the root of this specific anxiety
Being able to positively identify the circumstances that have triggered your anxiety (for example seeing others wearing masks reminding you of past time spent in hospital), and simply reminding yourself that you are not there now; instead mindfully noticing all that is currently around you, can be a helpful strategy for some. By identifying the trigger you can begin to understand the response, and you can positively remind yourself that you are no longer in that place – right now, you are safe. Tell yourself this.
Develop healthy habits
Developing and maintaining positive healthy habits is an excellent way to reduce anxiety in general, although not necessarily mask specific. Establishing healthy sleeping and eating routines, exercising and minimising caffeine and alcohol intake can all contribute to positive mental health.
Make it more ‘you’
Consider wearing a mask with a pattern or a pleasing colour. This will differentiate it from the sterile medical masks that may cause us to re-live past medical traumas. Perhaps pick a pattern that reflects your personality or interests, and try to focus on this positive. By personalising or ‘owning’ the mask, you just might feel more positive and in control of it.
How brainstrust can help
We are running a series of free to access live webinars on a comprehensive range of topics that you’ve told us are important to you if you’re living with a brain tumour diagnosis. You’ll find webinars on topics that will support you in managing anxiety, such as our hypnotherapy series that uses a blend of psychology and neuroscience to offer you practical tools to manage anxiety; or our nutrition programme to help support your overall physical and mental health.
Keep your community safe, protect yourself and your loved ones and represent the brain tumour community in a brainstrust face covering
brainstrust face covering – £6.99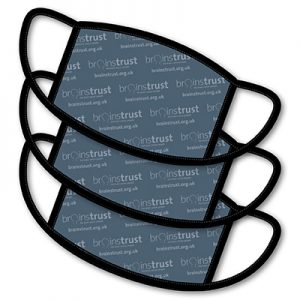
A machine washable, comfortable cotton mask, perfect for heading to the shops or when on public transport.
brainstrust face covering bundle – £18
A set of three brainstrust face masks, ideal so you always have one handy when others are in the wash. This bundle saves you £3.
brainstrust neck warmer – £11.99
This neck warmer is practical, easy to remove and can be worn in several different ways. Perfect for shopping and public transport but also for running, cycling and other outdoor activities too.









