Clinical Research: putting patients at the centre
People living with a brain tumour should come first. This is a core value for us, and it’s what sets us apart. We do our own research, which always starts with listening to what our community needs, and then we use this as a driver for change.
We don’t think that researchers should be concentrating on things that don’t matter to you. And we know what matters to you. A good quality of life, for instance, matters to you.
On this page you will find:
Ensuring the voice of patients is heard in research
We know that there is disconnect in the epidemiology (how and why a disease happens) of disease (clinicians) and epidemiology of healthcare (patients). Researchers tend to focus on progression free survival and overall survival; patients and carers focus on the quality of life issues like function and symptom relief. It’s the clinician’s role to explore and share what is possible and the patient’s role to explore and share their preferences and what they value. So we work with our community to bridge this gap.
We share agendas, represent patient voice and look for solutions.
Helping clinicians put patients at the centre of research
Clinical trials
We know that our community wants to engage in research. We know too that when patients see a clinical trial as important they are more likely to participate. And we know that when patients and carers are involved in trial design then the research has patient relevance, asks the right question and accruals to the trial are better. We have produced a guide for clinicians on how and when they can involve patients in clinical trials. We also run workshops for clinicians on how to involve patients in trials and how to write lay summaries.
Just like in all of our work, we’re committed to representing the brain cancer community voice in trials too. Through our presence on national bodies such as the NCRI Brain and CNS Clinical Studies Group, and the Commissioning Reference Group, we are able to keep ahead of open trials and feed this information into our brain tumour hub. We are also co-applicants with clinicians in trials which are exploring new treatments and quality of life. This means that we can keep ahead of the curve and know what is coming up so that we can share it with you, our community.
Growing an effective clinical community
We’re also improving patient outcomes by facilitating effective collaboration between clinicians who work in different specialties. To do this we have grown an enthusiastic clinical community that is really engaged with areas such as the neuro-rehabilitation and psychological agenda.
To find out more please email helen@brainstrust.org.uk.
If there’s one thing that researchers need to find a cure for brain tumours, it’s a sample of your brain tumour. Ask about tissue donation today.
Our own research, driven by the needs of patients
Have a look at some of the posters below, which we have presented at international and national conferences.
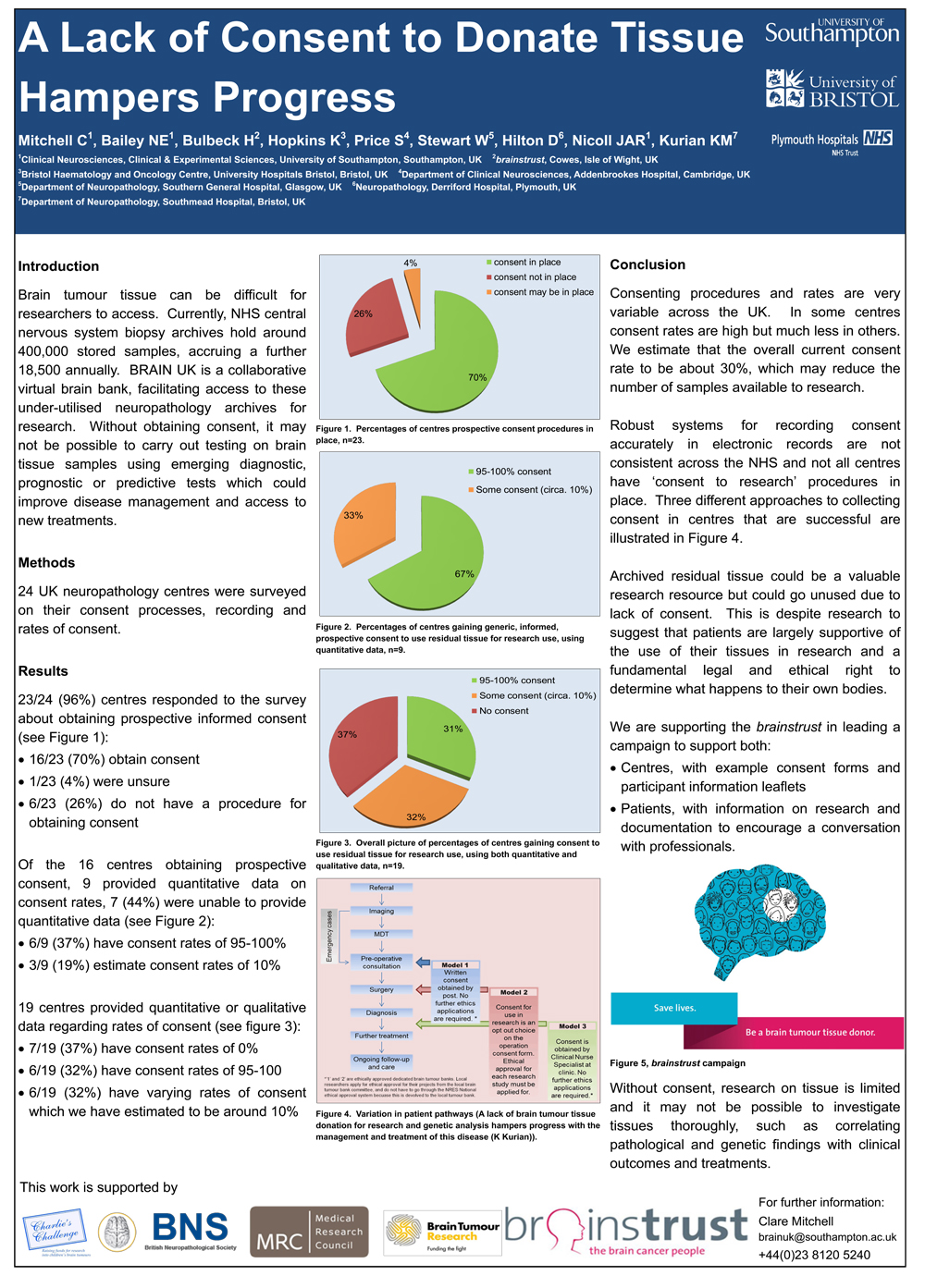
A lack of brain tumour tissue hampers research progress
Brain tumour tissue can be hard to access so brainstrust has been working with clinicians to unlock this resource.
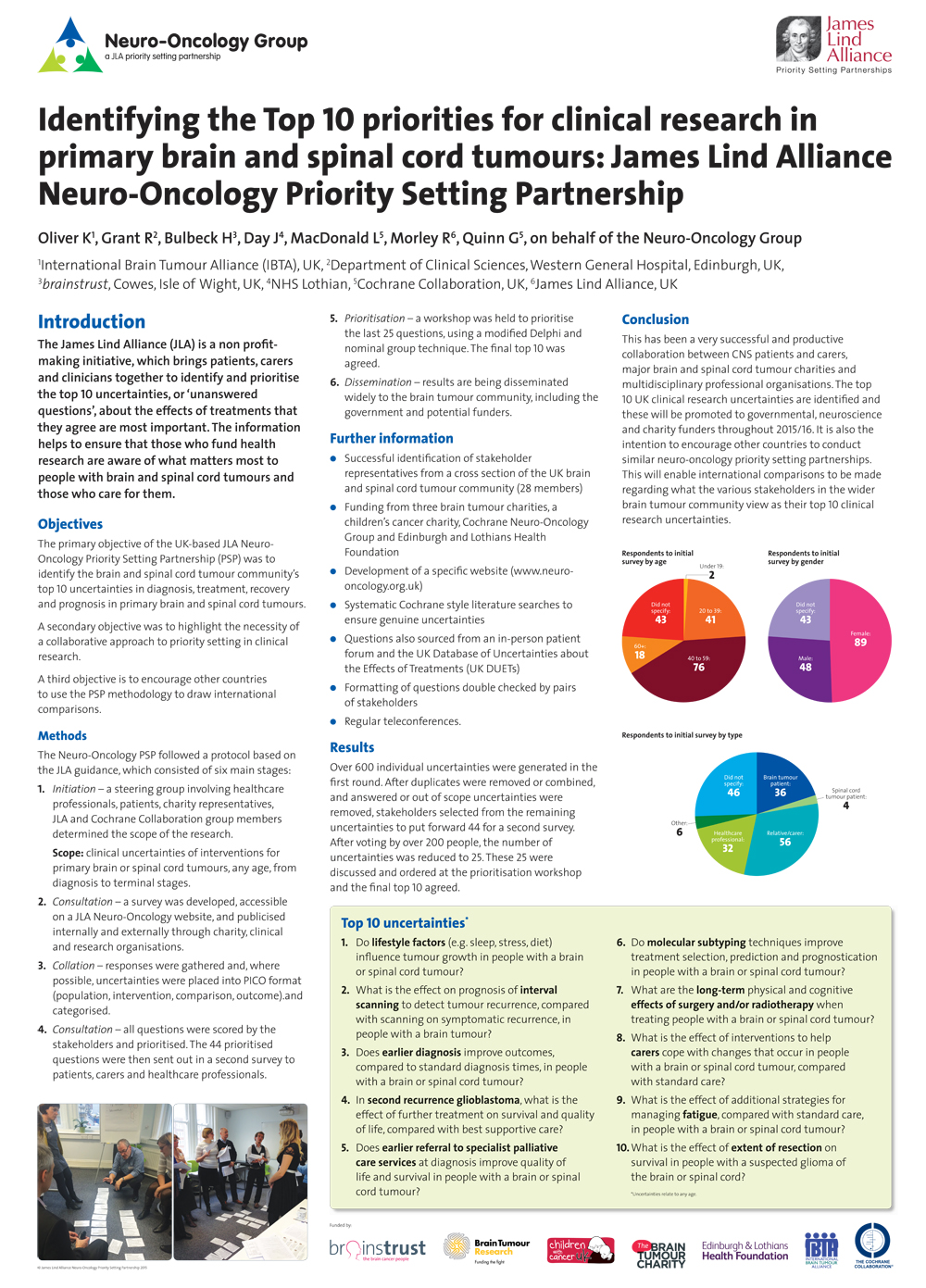
Top 10 priorities for research in brain cancer
The brain tumour community has worked collaboratively to identify the Top 10 priorities for clinical research.
neuro-oncology.org.uk
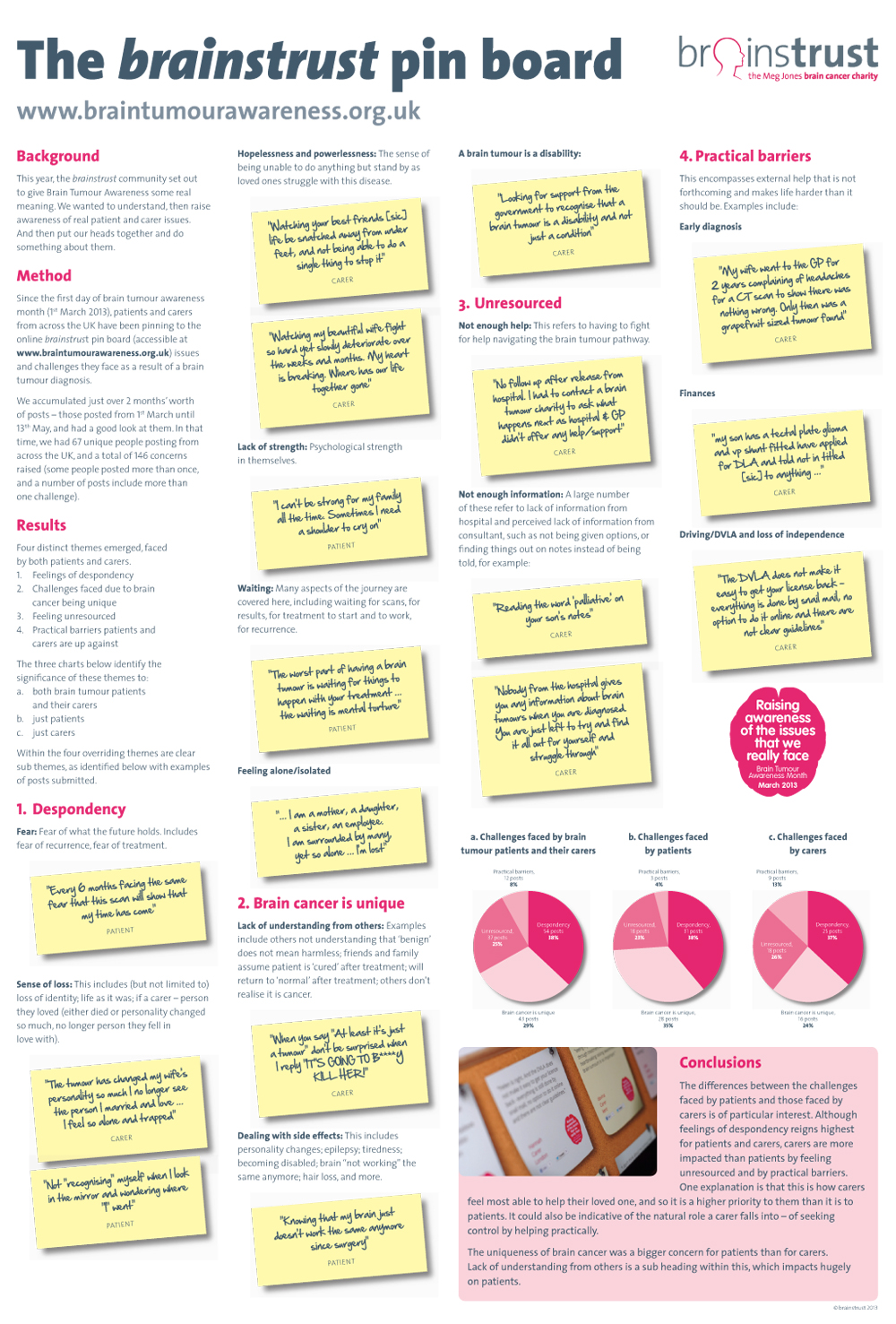
Share Aware Pinboard
The brainstrust community set out to give Brain Tumour Awareness some real meaning. We wanted to understand, then raise awareness of real patient and carer issues. braintumourawareness.org.uk
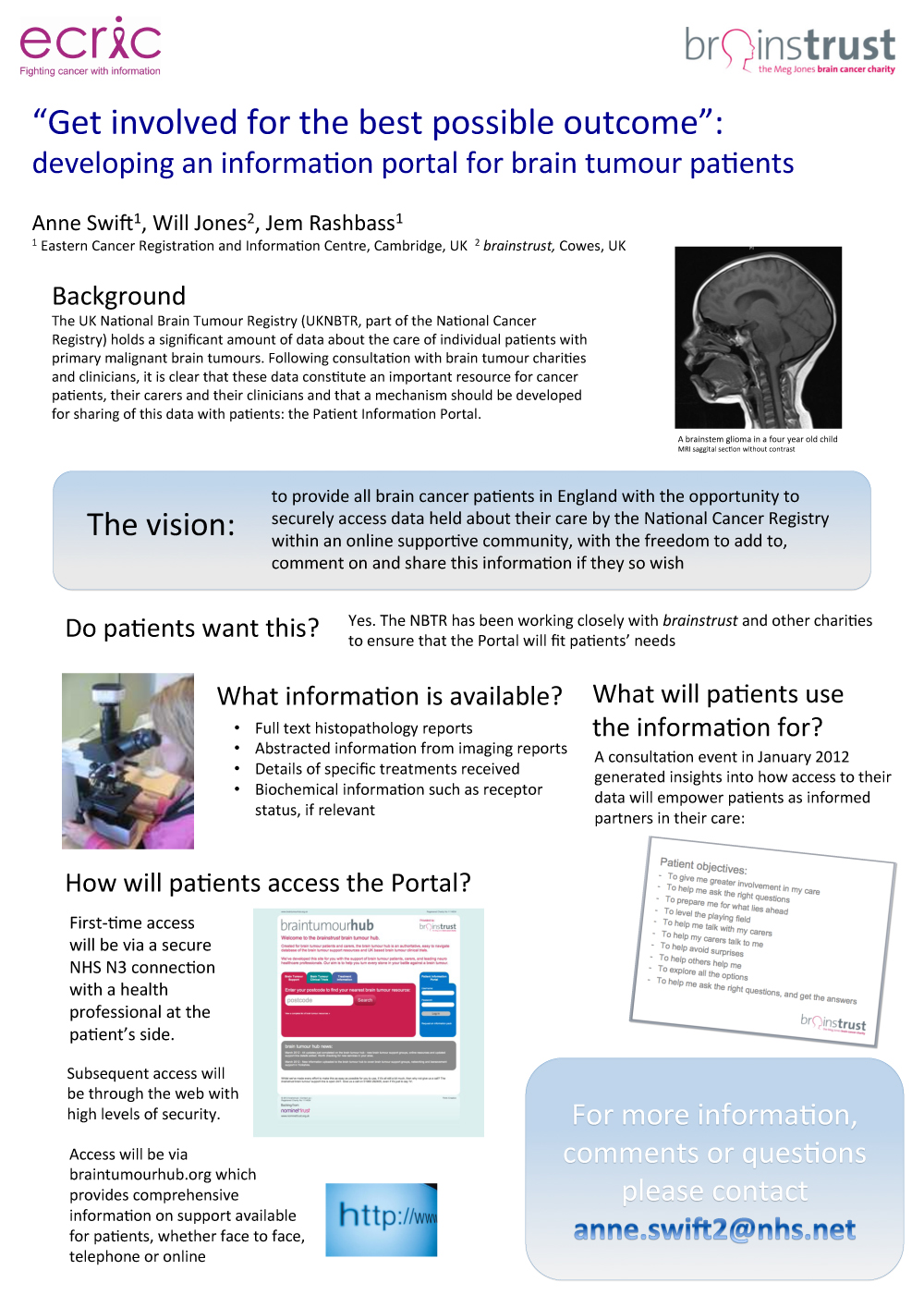
Patient Information Portal
Get involved for the best possible outcome: developing an information portal for brain tumour patients.
Campaigning to make clinical research the priority
Alongside basic science research not always having an impact upon the lives of patients, there are other reasons why we want to focus our attention on effective clinical research. Other leading charities, like CRUK and the MRC, fund basic science research and are currently investing in brain cancer more so than other cancers. Why would we put all our efforts into this type of research when it’s already being done and might not deliver results anyway? We’d be back at square one.
The other reason is controversial. We (along with some clinicians) don’t think you can find a cure for brain cancer, or even for any cancer. But what we can find is a way where people living with a brain tumour do so for a very long time, AND with a good quality of life – an exceptional quality of life and one that will prolong survival.
If we stopped looking for a cure and just focused on achieving a good quality of life for a long time as a goal, we’d win so much more ground.
How you can help us put patients at the centre of research
Join brainstrust’s campaign for better brain tumour research by:
- Sharing your experiences
Share your challenges and what you’d like to see improved during treatment. With this information we can ensure that research is meeting your needs. - Consenting to donate your brain tumour tissue to research
Visit The Brain Tumour Tissue Campaign page and see how starting a simple conversation could save lives in the future. - Fundraising
Support research that will make a real difference to the lives of patients and carers by joining an event, hosting a fundraiser or making a donation.
Together we can ensure that research is focusing on the things that matter to you.
Latest research news
14th April 2015 – Launch of our new report – Quality of life: what the brain cancer community needs. Read about how we’re making changes to the delivery of neuro-rehabilitation.