Preparing for Neurosurgery – A Timeline
Two to four weeks before your brain surgery
If you have been given a scheduled date for your surgery, you will have time to prepare and plan some practical coping strategies. By taking this time prior to your surgery, this will enable you to focus on healing after your operation, rather than worrying about daily responsibilities. Making choices will also help you to adjust to the uncertainty that living with a brain tumour diagnosis comes with.
surgery, this will enable you to focus on healing after your operation, rather than worrying about daily responsibilities. Making choices will also help you to adjust to the uncertainty that living with a brain tumour diagnosis comes with.
Often when faced with the prospect of surgery and feeling like you have lots to do, it can feel that you have to do everything yourself. Ask yourself, ‘who is in my team?’, and you will be able to come up with a list of people who you can go to for help and support. When asking people for support, it can be helpful to make specific requests such as ‘Could you take me to my appointment on Thursday?’ or ‘Would you mind taking this to the post office for me?’
Our Know How ‘Dealing with the overwhelm’ contains some useful tips and strategies that will help you during this time if you feel overwhelmed preparing for your surgery.
If you are struggling with the prospect of asking others for help or don’t know who to ask, our Know How ‘How to build a supportive team around you’ is full of tips and strategies for you to read and try.
Here are some more practical tips about ways to help you to prepare in the build up to your surgery date:
- Cook and freeze some meals and ask friends and family to provide you with nutritional food during your recovery. They will be only too pleased to be able to help and will be wondering what they can do to support you.
- If you are feeling well, catch up with some of the household chores so you won’t be looking at them when you come home. You certainly won’t feel like doing them after surgery.
- Buy any cards and presents that are needed for birthdays etc so that you can send them whilst you are recuperating.
- Make a list of films/TV shows that you want to watch and books you want to read during your recuperation. It may take a few weeks for your vision to settle down, if your sight is affected, but you will be able to read and watch for short periods.
- Plan for any childcare that you may require, or if you are looking after an elderly person.
- If you are working, you have time to make arrangements for any cover that you might need. You can delegate tasks and handover your workload so that you do not have to worry about this. This will speed up your recovery.
- It is tempting to avoid this subject, but it is a good idea during this period to review any personal documentation such as advance directives or Living Wills. This is a legal document which specifies which treatments you would like to have (or not) if you are unable to communicate your wishes with others. Or you might decide to designate a person who has power of attorney for health care, if you are unable to make medical decisions for yourself. This means that you have an assurance that your personal wishes will be respected in the event you cannot communicate. Our Know How about lasting power of attorney has more information.
One week before brain surgery
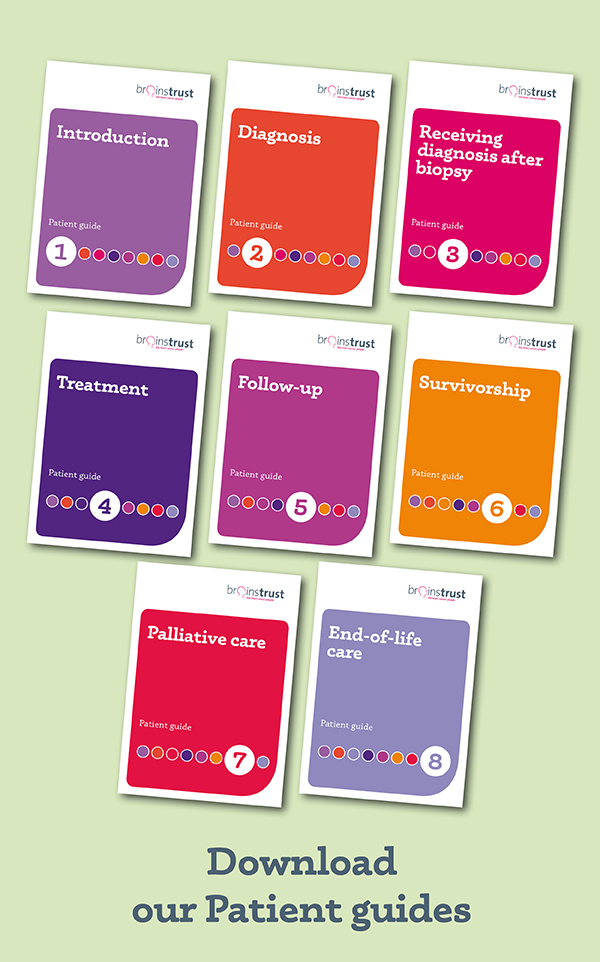
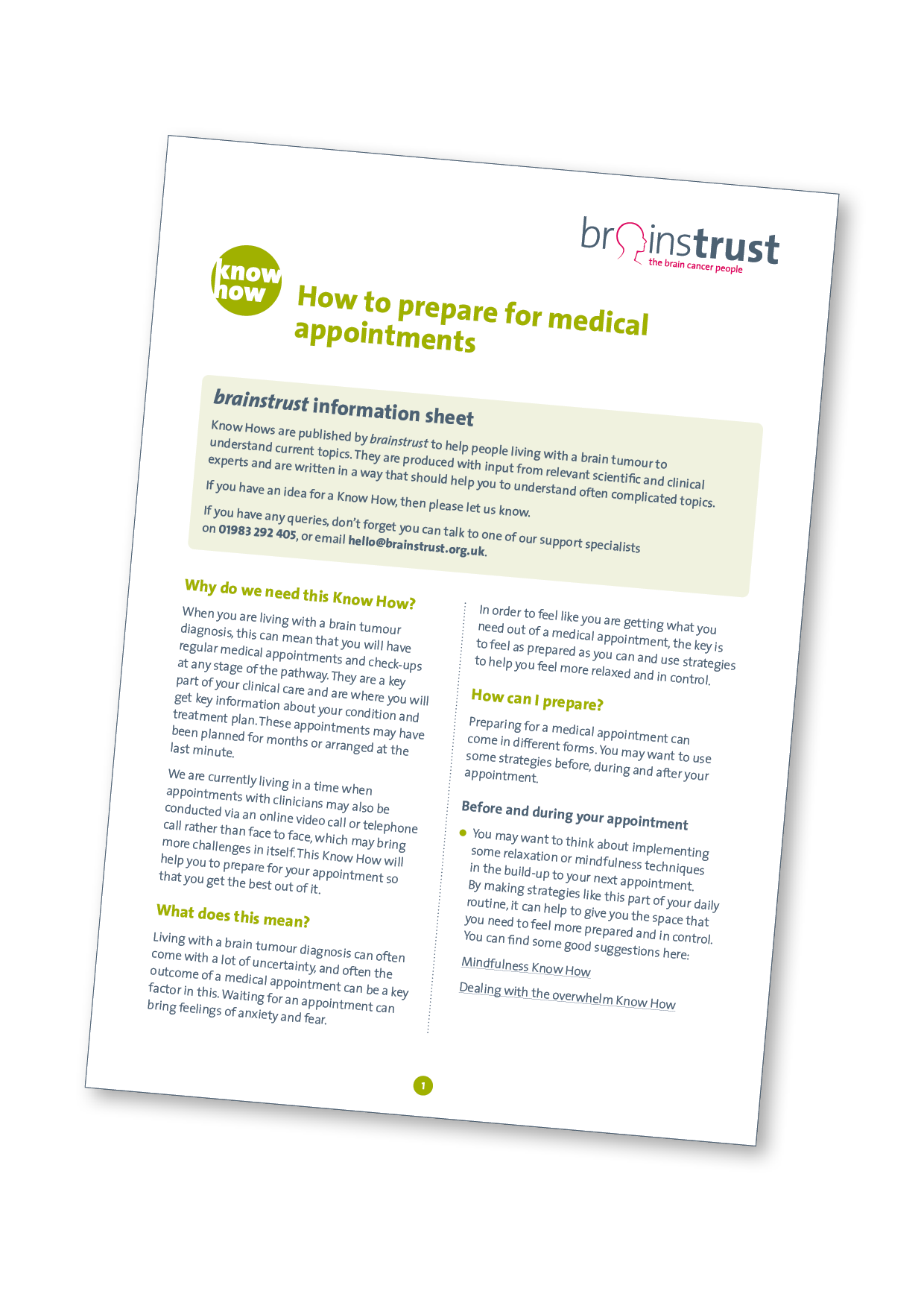 As the date approaches you will be anxious. Make a list of any questions or concerns that you still have. You will probably have to attend an appointment during this week where any preoperative tests will be done, such as an MRI, ECG, blood tests etc. You will probably have an interview with the anaesthesiology staff, and your medical history will be taken. Don’t forget to ask about taking any medication with you. Make notes; it may help if you can take someone with you for this appointment. Our Know How about how to prepare for medical appointments has more information that will help you to feel prepared.
As the date approaches you will be anxious. Make a list of any questions or concerns that you still have. You will probably have to attend an appointment during this week where any preoperative tests will be done, such as an MRI, ECG, blood tests etc. You will probably have an interview with the anaesthesiology staff, and your medical history will be taken. Don’t forget to ask about taking any medication with you. Make notes; it may help if you can take someone with you for this appointment. Our Know How about how to prepare for medical appointments has more information that will help you to feel prepared.
You will also need to reassure those around you. This may seem an odd thing to say, but they will be as worried as you are. Keep talking about what is ahead of you and also what you plan to do to celebrate when you come home. Allow time during this week to spend time with friends and family. Do some enjoyable things to alleviate the anxiety, which you will all be feeling.
Clarify with the hospital how family will be kept informed during the actual surgery. And ask someone in your family to take the responsibility of keeping friends and family informed.
You will be provided with a list of things to bring in with you, so make sure that you have a small bag. Take this time to gather together everything you will need to bring so you have time to get anything that you might not have.
This list should include:
- Any insurance documentation (if appropriate)
- Any prescription medication
- Glasses, hearing aids, dentures (if appropriate)
- Lightweight robe, slippers, nightdress or pyjamas. As your head will be bandaged, make sure that any tops are front closing so that you don’t have to pull them over your head. Choose clothing with short or wide sleeves (it is hot in hospitals) because of IV drips. Include one pair of socks.
- Personal toiletries.
- A small notebook and pen. Useful for key contact numbers, noting milestones in your recovery, questions that bug you at 3am.
- An inexpensive watch – this is important. Your routine is about to be turned upside down, starting with a very long, blissful sleep (if you are not having an awake craniotomy) and you will find it comforting to know what the time is so that you can have some structure to your day.
- You might want to take some pictures of your family and friends to look at and some light reading.
- Small change will be invaluable.
- Mobile phone/tablet charger.
Know how to talk with your neurosurgeon about tissue collection
When you are having surgery for a brain tumour, it is important that you talk with your neurosurgeon about what will happen to the tumour tissue that is removed.
tumour tissue that is removed.
This know how will help you to understand the options available and the things you need to think about.
Download the tissue collection know how
The surgery day
You may be admitted the day before or early on the day itself. It will be long day for everyone involved and sooner you get on with the it the sooner it will be over. You won’t know much about it! You will not have been able to have eaten anything since the previous midnight, but you will able to rinse your mouth with water without drinking.
You will change out of your clothes and be asked to put on a surgical gown. Ask for help if this defeats you! Don’t wear jewellery (although wedding rings can be taped on), contact lenses, dentures and remove make up and nail polish – the doctor needs to see your toes and fingers to make sure they aren’t blue.
You may be given a pre-med which is great – it relaxes you and takes the stress out of the situation. An IV line may be inserted before you go to theatre, but the bulk of the invasive work is done after you have been sedated, so you won’t know anything about it.
After your surgery you will be taken to recovery or directly to an intensive care unit (ICU). When your pulse, blood pressure, temperature and other vital signs are stable you will be moved to another area where you can be monitored closely for 24 hours. You can read more about what happens after surgery here.
Did this information make you feel more resourced, more confident or more in control?
Date published: 17-05-2009
Last edited: 05-2025
Due for review: 05-2028