End-of-life care for people with a brain tumour
“It is difficult to exaggerate the importance of good end-of-life care. After all, we only ever have one chance to get it right.”
Death is the one sure certainty for us all, yet we rarely discuss end-of-life care and what our final wishes would be. Having all the relevant information allows you to begin the conversation, make sure any requests are in place and ensure that you feel in control.
Our ‘End-of-life care’ resource has been produced with people who have the lived experience of what it is like to care for someone with a brain tumour at end-of-life, with leading consultants in palliative care and clinical nurse specialists who are hospice-based.
It covers all aspects of what dying with a brain tumour entails. This resource provides information on good end-of-life care, how to achieve it, who can help you and how to ensure that you are being informed and making the right decisions that are personal to you. It will take you through options for stopping treatment through to looking at making decisions for where the patient wants to die. Having as much information to hand as possible allows you to be in control, certain that you are making the right decisions for those concerned.
On this page you will find:
Coaching with brainstrust
Coaching with one of our support specialists can help you understand what’s important to you, so you can start having the conversations you need to live the best day possible, every day. Book a session today to start your journey from panicked to prepared.
The brainstrust end-of-life care resource
With our EOLC resource you will:
- have independent, factual information available on EOLC when living with a brain tumour for patients, caregivers and stakeholders
- have the information you need so that you can make informed decisions about EOLC and how to manage it
- understand what happens in EOLC quickly and easily, with evidence supporting the information
- be able to build trust in clinical judgement and in stakeholder decisions
- be able to articulate the challenges around EOLC so that you can be more open in your discussions.
Click here to download the complete EOLC resource.
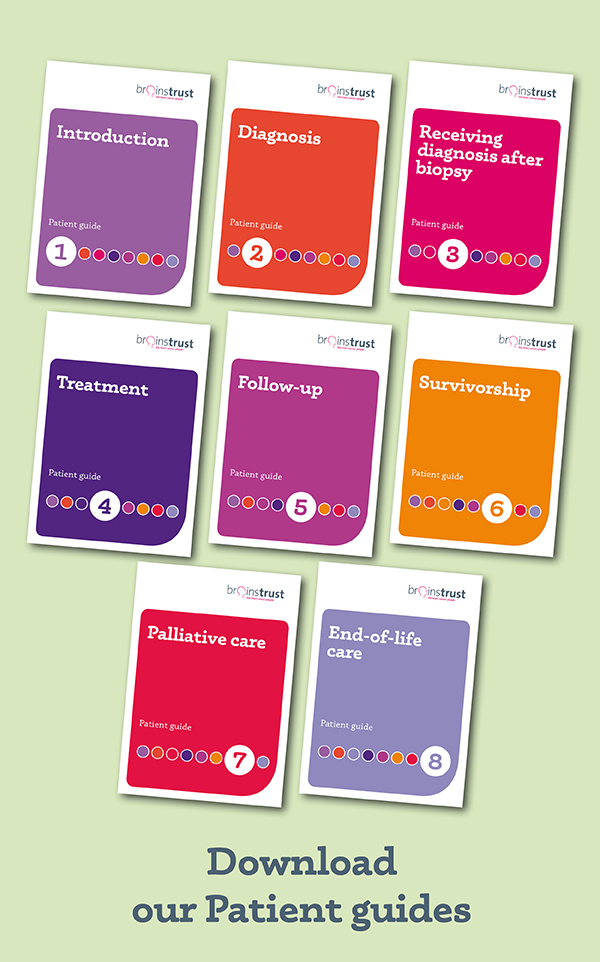
The resource is split into six downloadable sections, which you can access below. If you would like a hard-copy of the resource, please email hello@brainstrust.org.uk and we will send one out to you.
The difference it makes
“How we die lives on in the memory of those left behind.” Dame Cecily Saunders
You need people to hold you through this, not necessarily to understand it, and this is what this resource is planned to do. With planning, the right conversations at the right time, and with the right support, we believe that you can still have your best possible day, even at end-of-life. This resource and our support will enable this to happen.
Here, our support specialist for Scotland Carol reflects on the difference that talking about death and planning end-of-life care made for her family:
“Death is the great one certainty for us all, yet it’s still such a taboo subject. It’s so important to be having conversations about it as it alleviates the fear. It gives the opportunity to make sure you know the dying person’s wishes are met, but it’s more than that.
When my Dad was diagnosed with a glioblastoma we used it as an opportunity not just to ensure his end-of-life care wishes were met (he wanted to die at home), but to use the time to make precious memories as a family with the time we had left, as we knew time was such a precious commodity.
Knowing we did this helped greatly after Dad died – knowing we had those conversations, nothing was left unsaid, and we had a treasure trove of memories made.”
At some point in the course of a malignant brain tumour, it is likely that treatment options will run out. Supportive care should become the focus. But this sounds easier than it is.
Some patients prefer to stop treatment and let the disease take its course. This should be respected but is not irreversible if the patient changes their mind. The focus should always be on the goals and priorities of care; this should define the type of treatment and helps with decision-making.
For more information, read Part 2 of the End-of-life Care resource, page 16.
You can ask for help at any point you feel out of your depth, you feel overwhelmed or upset. How to find the support you want and the questions to ask are outlined in Part 3 of the End-of-life Care resource, page 31.
In our experience, which is based here on talking with many carers, the person with brain cancer can remain stable for a while but then deterioration happens very quickly, sometimes over a matter of hours.
For more information on brain cancer progression, read Part 5 of the End-of-life Care resource, page 45.
Instinct will tell you. At the point of death breathing ceases completely, and there is no detectable pulse. Take a deep breath, and have some quiet moments of calm. Your loved one is at peace. There is no rush to act now.
For more information, read Part 5 of the End-of-life Care resource, page 58.
For support in coping with bereavement, click here.
Sources used in writing this page
National Council for Palliative Care
Clinical Nurse Specialist
Caregivers
Consultant in palliative and end of life care
NICE. 2019 End of life care for adults: NICE guideline [NG142]. London: NICE. London: NICE [Accessed 10 September 2021].
NICE. 2021 End of life care for adults Quality standard [QS13]. London: NICE.[Accessed 10 September 2021].
NICE. 2021 Brain tumours (primary) and brain metastases in adults: NICE guideline [NG99]. London: NICE [Accessed 10 September 2021].
Did this information make you feel more resourced, more confident or more in control?
Date published: 09-2021
Last edited: 08-2025
Due for review: 02-2028
Help fund our mission
92%* of people told us that this information has helped them feel more resourced and in control.
A donation of £3 a month helps us keep this information up to date.
*579 out of 627 respondents
Subscribe to our mailing list to hear about all the latest news, events, research and resources.