Brain tumour symptoms and diagnosis
On this page, you will find information about brain tumour symptoms and how a brain tumour diagnosis is made. You will also find further information to support you in navigating your clinical care and to help you feel better resourced.
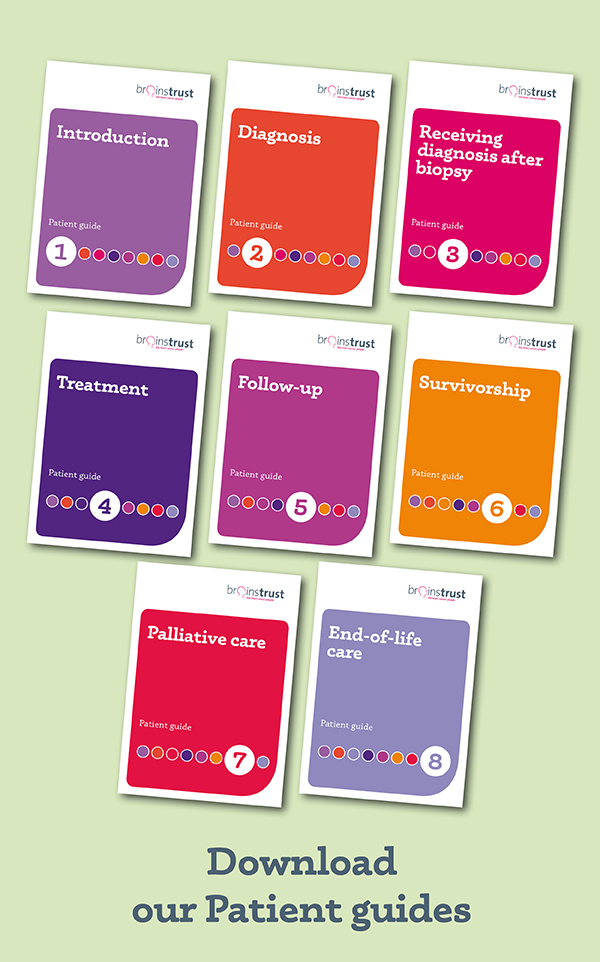
Read the diagnosis section of our patient guide for further guidance.
On this page you will find:
Brain tumour symptoms & signs
Doctors refer to brain tumour symptoms and signs.
- Symptoms are abnormal changes you have felt.
- Signs are what other people have observed about you e.g. that you have a weakness in an arm or leg or are having difficulty with speech.
Because there are so many different types of brain tumour, there are a number of brain tumour symptoms and signs, depending on the nature of the brain tumour and where it is. These may be very severe, or may not be apparent at all. So, it is a very broad spectrum with which we are dealing. Please remember this if you haven’t been diagnosed with a brain tumour. It is a rare condition and having a headache for more than a week does not mean that you necessarily have a brain tumour.
Brain tumour symptoms
| Symptom | Comment |
| Headaches | Headaches which are more severe in the morning and wake you in the night. They are usually different from headaches you might have had previously and will be persistent and worsen with time |
| Nausea and vomiting | With a headache this can indicate increased pressure in the head (raised intracranial pressure). |
| Seizures | A seizure is abnormal electrical impulses in the brain, causing sudden involuntary changes in movement or function, sensation, awareness, or behaviour. A first time seizure in an adult is often investigated. |
| Weakness, loss of sensation or numbness | This is a sign of pressure on (or damage to) a specific part of the brain and can also be manifested through walking unsteadily or lack of coordination (ataxia) or muscle weakness on one side of the body (hemiparesis). |
| Hearing loss | Could be a sign of an acoustic neuroma if it occurs only on one side. |
| Loss/disturbance of vision, including double vision | In one or both eyes could be a symptom, if there is a tumour pressing on the optic nerve or there is one affecting the visual pathways or if there is raised intracranial pressure. |
| Speech difficulties | May also include the loss of ability to write, speak or understand words. A person may have difficulty getting the right words out (expressive dysphasia) or difficulty articulating them (dysarthia). |
| Other brain tumour symptoms | Lack of concentration, confusion, memory loss, disorientation, drowsiness, change in behaviour. |
Coaching with brainstrust
We know a brain tumour diagnosis can leave you feeling overwhelmed and frightened, stranded in a strange and lonely new world. As coaches we listen to you, listen some more, and then ask questions to help you understand what it is you need and how you can plan to achieve those goals. Book your first coaching session today and start taking control.
Brain tumour diagnosis
When you hear the words “you may have a brain tumour” it can be a terrifying, isolating time, causing uncertainty.
This ‘What to expect if you are diagnosed with a suspected brain tumour’ leaflet will help you to cope with the fear and uncertainty. It explains what you can expect to happen next, so you can feel more informed and more in control after your scans. We’ve also included some top tips from those that have been through the same experience.
How a brain tumour diagnosis is made
The bones of the skull hide brain tumours. You cannot feel or see them during a routine examination. Scans produce pictures that suggest a particular type of tumour. But the only reliable way to an accurate diagnosis is to examine a sample of a tumour under a microscope; this is called a biopsy, so a biopsy will sometimes need to be done. If this type of examination is not possible, an educated assumption is made based on available test results.
If there is a suspicion that there might be a brain tumour, then your doctor has a whole host of diagnostic weaponry, which will aid an accurate diagnosis. These tests determine firstly whether you have a brain tumour and then, if you do, what type of tumour.
MRI scan – magnetic resonance imaging. This uses magnetic and radio waves, so no exposure to X-rays or any damaging forms of radiation. An MRI scan takes pictures from any direction. Contrast agents (usually gadolinium) can be used to outline the lesion. These are usually injected into a vein in the arm during the scan. Sometimes the agent can make you feel a bit sick.
Just a word about pacemakers; you may not be able to have an MRI scan if you have a pacemaker fitted or other metal objects in your body but alternatives are offered. Some new pacemakers are MRI compatible though – you will need to check with your cardiologist.
The scan will last about 45 minutes and can be noisy. Some hospitals let you listen to a CD so take one just in case.
Other tips – wear warm clothing; it can be chilly in the room. You will need to take off jewellery and anything else metal. This includes underwired bras and jeans with studs in.
If you have a child undergoing an MRI scan, get them to imagine they are going into a space capsule.
You should receive the results within two weeks. Privately, you can have the scan and reporting done on the same day, but private scans can be expensive. The costs of private MRI scans can vary depending on hospital and geographical location. If you do decide to have a private scan you will need to make sure that the cost of having the scan read by a neuroradiologist is also included.
CT scan – computerised tomography. Instead of sending out a single x-ray through the body, several beams are sent simultaneously from different angles. The computer then processes the results showing them as a 2D picture. CT scans are less expensive and take less time than an MRI scan, but they have lower resolution so could potentially not show some skull base and low grade tumours as well as an MRI scan. So, if you have one type of scan rather than another, it is usually because one will be more suited to you.
A CT scan usually lasts around 20 minutes and is quieter than an MRI scan. You lie on a table and the scanner moves around your head. If you need a contrast scan, then an iodine-based contrast agent will be injected. This shows the ‘leaky’ blood vessels in a tumour and enables the neuroradiologist to see the mass directly.
Other tips – Warm clothing is recommended; it can be chilly in the room. And if you are allergic to shellfish let the radiographer know, because some contrast agents contain iodine.
Reporting is usually done within two weeks. Again – this may be sooner if you have a private CT scan.
PET scan – position emission tomography. Only a few hospitals in the UK have a PET scanner. This too produces a 3D image but in colour. The patient is given radiation via a medicine called a radiotracer. This goes to the part of the body that needs to be examined. The PET scan then detects radiation inside the body and makes images that show how the radiation is being broken down. This type of scan is not generally used to diagnose a brain tumour, but it can provide additional information about the nature of the tumour. For example, it may help to determine the difference between a non malignant and malignant tumour because malignant tumours are more metabolically active (that means that within the tumour cells that are alive and growing, chemical reactions are happening within them). And it can show the effects of treatment. For more information about the difference between non malignant and malignant tumours visit anatomy and tumour types.
The scan itself takes about 30 minutes. About 40 minutes before the scan you will be injected with a mildly radioactive substance which has no risk to the body as the level of radiation is very small.
SPECT – single photon emission computed tomography. Similar to PET, a SPECT scan views how blood flows through arteries and veins in the brain. It differs though from a PET scan in that the chemical stays in your blood stream rather than being absorbed by surrounding tissues, thereby limiting the images to areas where blood flows. SPECT scans are cheaper and more readily available than higher resolution PET scans.
As with the PET scan, an injection of a small amount of radioactive tracer is given prior to the scan. Then you’ll be asked to rest for about 10-20 minutes until the tracer reaches your brain. Next you’ll lie comfortably on a scanner table while a special camera rotates around your head. You have to remain as still as possible so that the machine can get accurate pictures.
Other tip: be sure to drink plenty of fluids to flush out any tracer left in your body.
Angiography – this shows the blood vessels in the brain – the arteries, the veins and sinuses. Angiography will not feel any different to having a CT or MRI scan if it is done as a CT or MRI angiogram.
It can also be done with an injection of iodine dye into the femoral artery in the groin, which is then threaded through to the brain. This sounds worse than it is; a numbing agent is used and you may feel brief pain when the catheter is inserted. Sedation is sometimes given for this test.
You will feel a hot, flushed sensation lasting from 5 to 20 seconds as the images are taken. This may be repeated several times in order to view all necessary arteries, so this test can last several hours. You will need to be careful afterwards to prevent bleeding. In some instances, a puncture closure may be used which will allow you to get up and move around sooner.
Any invasive test carries risk. There is a very small risk of the catheter damaging your artery or loosening a piece of plaque lining the artery wall. And then there is the risk of sensitivity to the contrast agent used. The most common side effects from the iodine contrast are a brief metallic taste in your mouth and a feeling of warmth throughout your body.
Brain tumour fatigue is so much more than ‘feeling tired’. We know. Learn how to manage fatigue here.
Brain tumour biopsy
In some cases, if a diagnosis cannot be made clearly from the scans, a biopsy may be performed to determine what type of tumour is present. A biopsy is a procedure to remove a small amount of tumour to be examined by a pathologist under a microscope. A biopsy can be taken as part of an open surgical procedure to remove the tumour or as a separate diagnostic procedure, known as a needle biopsy via a small hole drilled in the skull. A hollow needle is guided into the tumour and a tissue sample is removed. There are different ways of doing a biopsy, but not all will be available. It depends on the technology and experience that the neurosurgical centre has. As with all invasive surgery, a biopsy carries a small amount of risk, but it is small. Over 95% of biopsies are successful in obtaining the sample of tissue sufficient to give an accurate diagnosis. Surgery will usually last between ½ and 2 hours.
Having a biopsy will provide a more accurate diagnosis. With advances too in the biology of cancer, the results of your biopsy can also help map out the best treatment pathway for you. Your tumour tissue will be examined by a neuropathologist. They determine what type of tumour it is you have (and it can be one of about 140) and will play a key role in the Multi Disciplinary Team (MDT) meeting about what the options are for your treatment.
Once a biopsy is done, your brain tumour will be the focus of an intensive investigation using all sorts of complex tests. Increasingly, this may include an exploration of its genetic profile so that as accurate a diagnosis as possible can be formed and the right therapies can be matched to your need; guiding your treatment so that it is optimised for you. For more information on these tests read our page on therapies and treatments for a brain tumour.
Other tests you might be offered
Hearing tests – audiometry. A hearing test, performed by an audiologist, detects whether hearing loss is due to a bone (conduction) problem or nerve damage, which is caused by pressure from something, such as a tumour near the cochlear nerve (e.g. acoustic neuroma). These are completely painless, lasts about 30 minutes.
Visual field tests – perimetry. This can be performed by an optician or a neuro-ophthalmologist to detect vision loss and missing areas in your field of view. It takes little time (20/30 minutes) and is completely painless. Results are usually available immediately.
EEG – electroencephalography. Our brains are full of electrical activity and so an EEG records this activity: the absence of, as well as areas of abnormal activity, seen in epilepsy. The only discomfort you will feel with this is a bad hair day. The electrodes are attached to your scalp using a sticky gel – this is the longest part of the whole test. The actual test can take anything from 20 minutes up to two hours. After the test your results will need analysing so this may take a few days.
Other tip – don’t put gel or hair products on your hair the day you have this done. This may prevent the electrodes sticking.
Endocrine evaluation measures hormone levels in your blood or urine to detect abnormal levels caused by pituitary tumours (e.g., Cushing’s Disease).
A lumbar puncture (spinal tap) may be performed to examine cerebrospinal fluid for tumour cells, proteins, infection, and blood. This involves placing a needle into the lower back during a procedure which lasts about 20 minutes. There may be some local discomfort and after the procedure you may have a headache, but you should be encouraged to lie flat after the procedure to build up the fluid, which has been removed.
Glossary
Some words you might hear during the diagnosis stage of your journey
artifact: images on an MRI scan that may be caused by movement during the scan, metal or a processing problem
coronal image: an MRI image which splits the brain into front and back sections
decreased signal: objects that appear darker on an MRI scan
enhanced MRI; an MRI after contrast, such as gadolinium, is given
gamma rays: electromagnetic radiation emitted during radioactive decay and having an extremely short wavelength
increased signal: objects that appear whiter on an MRI scan
photon: a particle that travels at the speed of light
positron emission tomography (PET): a nuclear medicine test in which tissue function is imaged. Damaged tissues have reduced metabolic activity, therefore gamma radiation from these areas is reduced or absent
positron: an electrically charged particle that has the opposite charge as an electron. It reacts with an electron to produce gamma rays.
radiolabel: the technique of attaching, or “tagging”, a radioactive molecule to another molecule (such as a protein) so that it can be identified in the body.
sagittal image: a sideways MRI image that splits the brain into left and right sections
tomography: the technique of using rotating X-rays to capture an image at a particular depth in the body, bringing those structures into sharp focus while blurring structures at other depths.
tracer: a substance, usually radioactively labelled, which is injected into your body and can be followed to gain information about metabolic processes.
Click here to view our full glossary of terms you might encounter on your brain tumour journey.
Brain tumour support is driven by your support. We know. Click here to help us do even more for people living with a brain tumour in your area.
Just been told?
Right now you will be in a state of shock – your world has been completely turned upside down. But there will come a point at which you will feel that you are in control of a situation over which you feel that you have no control – at the moment. It does get better.
What to do when you hear the diagnosis
Nothing can really prepare you for the news that you or someone you love has been diagnosed with a brain tumour. Whether you knew that something hadn’t been quite right for a while, or whether it was a sudden discovery, it tears at the warp and weft of your life; it changes everything. The route to receiving this diagnosis may look different for each person. However you come to receive your diagnosis, you will find yourself in the shock of the new, wondering what this means and what is next. You will be reeling but your ability to cope does get better – you develop systems to cope with such traumatic change.
What you want to know is that you have explored every avenue and have done everything that you can be doing to help. We can offer the following suggestions, but please remember we are not doctors. Much depends on where you are based and the mindset of the people with whom you are working.
Our suggestions
- Keep copious notes of everything, including a contact list of the people involved in your or your loved one’s care. Ask consultants to write to you afterwards about what was discussed. Not all do this automatically and make sure that the GP is copied into these letters. Our brain box includes ‘my brain book’ which has plenty of space for you to write notes and keep important information related to your care together. You can request a brain box to be sent to you, here.
- Obtain at least two sets of extra scans from the hospital. Some hospitals do charge a small amount for these (around £30), but most don’t. Keep one for yourself and take these along to consultations, for the same reason outlined above. Use the other to send for second, third opinions. Don’t be put off by a reluctance to let you have them. Insist, quietly and firmly.
- Technology changes so it doesn’t really matter where the MRIs (brain scans) are done. What is critical is to make sure that there is a dedicated neuroradiologist who reads your scans so that they know the state of play intimately. It won’t always be possible but if it is, insist on this too.
Ask who you can contact for further support or if you have any concerns. This will generally be a Clinical Nurse Specialist, but this can vary depending on hospital and area. Take a look at our Know How ‘Newly diagnosed- knowing what to ask’ for more information and tips to help you. You can find this here.
A word about seeking further opinions
We are mindful that everyone reacts to a serious diagnosis in different ways. It is your right to seek further opinions, and this will empower some people. Some people would prefer not to exercise this right. Some people prefer to know as little as possible about their diagnosis; some people like to relinquish control of their situation to others. All of these are perfectly normal and acceptable ways of coping. And seeking second, even third opinions can cause confusion and stress. But they can inform, and help with decision-making. They can also be reassuring. We believe that you need to be informed to make decisions. And that might mean gathering information and then deciding not to make a decision. That’s a decision too!
The key to this is knowing what your options are. And if you need to make doubly sure that the options you have on the table are the right ones for you then think about a second opinion. You also need to know that you may hear that there are no other options and this can be distressing. What is key is that you are in charge and that the path that you choose is the right one for you. Do not worry about upsetting your clinicians – a good clinician will understand the need to seek other opinions in a diagnosis as serious as this.
Read our Know How on second opinions
How to get a second opinion about your brain tumour diagnosis
If you want to seek further opinions, you will need a copy set of scans. Ask your hospital for these. There are two ways of seeking a second opinion:
Visit your GP and ask for a second, even third opinions. If you want more information about where you might go and who might be appropriate to see, ask us at brainstrust, ask your consultant or your GP. Get your GP on your side – they can unlock so much for you.
We can also help. Contact hello@brainstrust.org.uk. We can’t give you a second opinion, but we know someone who can – at one of the leading neurosurgical centres in the UK. You don’t always need to go through your GP for this.
Finally, you will be frustrated but don’t expect answers from your healthcare team, unless you ask the question. That’s why it is so important to be informed. Once you accept this you will be able to handle the whole situation much more effectively. Seek second, third, even fourth opinions and then try to stand back and draw out the key notes. Your position is not easy – you will be feeling like you are damned if you do and you’re damned if you don’t but at least you will be able to say that any decisions you have made have been informed decisions.
Knowledge is power: key questions to ask your doctors
I can’t honestly tell you what a weight this has lifted. I’ve been really alone since my last consultation as I feel like I’m burdening friends and family by discussing it over and over, but at the same time, it’s such a huge decision that I don’t want to make on my own. This consultation will honestly be amazing and will help me so much
Patient
It is essential to know about the type of tumour and also whereabouts it is in the brain, as this will provide information about the type of brain tumour symptoms that could be experienced. If possible seek the answers to these key questions as soon as you can:
- What is the brain tumour type?
- What grade is the brain tumour?
- Where is the brain tumour?
- How will its position impact on me?
And of course, the more you know, the more in control you will feel as you will be able to make informed decisions about which direction you should take whilst navigating your way around.
Your suggestions
The more we can sail this ship together the better. If you have any further ideas/advice you can share with us then please get in touch.
Resources used in writing this page:
brainstrust patient/caregiver representative
Consultant Neurosurgeon
Overview of the clinical features and diagnosis of brain tumors in adults
E Wong and J Wu, last accessed December 2024
EANO guidelines on the diagnosis and treatment of diffuse gliomas of adulthood
M Weller and others
Nature Reviews Clinical Oncology, 2021 Volume 18, Pages 170 – 186
Brain tumours (primary) and brain metastases in adults
The National Institute for Health and Care Excellence (NICE), July 2018
Living with a Brain Tumour (Peter Black) 2006
Fast Facts – Brain Tumors (Abrey and Mason) 2009
Primary Central Nervous System Tumors – pathogenesis and therapy (Current Clinical Oncology), Humana Press 2011
Did this information make you feel more resourced, more confident or more in control?
Date published: 17-05-2009
Last edited: 01-2025
Due for review: 01-2028
Help fund our mission
95%* of people told us that this information has helped them feel more resourced and in control.
A donation of £3 a month helps us keep this information up to date.
* 61 out of 64 of survey respondents