Many people with a brain tumour are not receiving the care and support they expect, according to the  National Cancer Patient Experience Survey 2016.
National Cancer Patient Experience Survey 2016.
The survey is designed to monitor national progress on cancer care, provide information that could be used to drive local quality improvements, assist multi-disciplinary teams, commissioners, and NHS Trusts in improving patient services, and inform the work of charities supporting cancer patients.
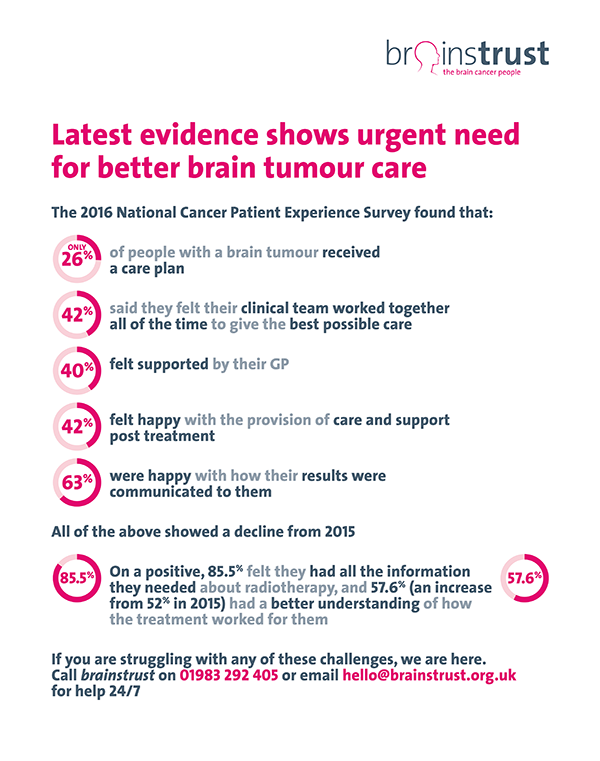
The survey found that:
• Only 26% of people with a brain tumour received a care plan
• 42% said they felt their clinical team worked together all of the time to give the best possible care
• 40% felt supported by their GP
• 42% felt happy with the provision of care and support post treatment
• 63% were happy with how their results were communicated to them
All of the above showed a decline from 2015.
• On a positive, 85.5% felt they had all the information they needed about radiotherapy, and 57.6% (an increase from 52% in 2015) had a better understanding of how the treatment worked for them.
At brainstrust we believe that everyone living with a brain tumour should receive the best possible care and treatment. We work with patients, their families, carers and health professionals to help them secure the right care for them.
We’re disappointed with the results from the 2016 survey and are committed to making sure the brain tumour community is better supported at all stages of their cancer journey.
brainstrust’s Helen Bulbeck, director of services and policy, said. “In the face of generally positive, and improving, experience (respondents gave an average rating of 8.7), brain tumour patients continue to be suffering unnecessarily, as evidenced by these eye watering results. Being diagnosed with a brain tumour is not like other cancers. Living with a brain tumour brings progressive neurological deficits and so there is far more at play, not least the 120 different types of brain tumour. With so many challenges presented by the tumour and the blood-brain barrier, and then the cognitive, physical and emotional impact, caused by the tumour and treatment, it’s easy to see it’s a serious disease with unmet need, both in terms of treatment and interventions around quality of life. We have made marginal gains, but the job is not done.”
Here’s what we’re doing
We know that things are not as good as they could be, that’s why we’re here.
- We’ll be talking with two professors of primary care for oncology and diagnostics to find out how patients and caregivers can be put back in control of their care and treatment.
- We will revisit our programme which explores how to have better conversations with clinicians.
- We will look into the barriers for the low accrual rates for brain cancer clinical trials, and continue to work with Cancer Research UK and The National Cancer Research Institute
- We will continue to focus on improving the transition point to community care after acute treatment.
We will keep working hard to ensure that everyone who is diagnosed with a brain tumour knows about the range and quality of our support. - We will continue to work with patients, their families and carers so they can have improved conversations with clinicians.
What you can do for a better experience
- Contact brainstrust to talk to one of our support specialists, who will be able to help and support you on your cancer journey. Call 01983 292 405 or email hello@brainstrust.org.uk
- Visit our support pages on the website for information about brain tumour treatment and care.
- Visit our events page www.meetup.com/brainstrust for details of our workshop, events and meet ups.
- Share your story with us. Help us raise awareness so that we can help more people living with a brain tumour. Call 01983 292 405 or email hello@brainstrust.org.uk