Second opinions
We are mindful that everyone reacts to a serious diagnosis in different ways. It is your right to seek further opinions, and this will empower some people. Some people would prefer not to exercise this right. Some people prefer to know as little as possible about their diagnosis; some people like to relinquish control of their situation to others. All of these are perfectly normal and acceptable ways of coping. And seeking second, even third opinions can cause confusion and stress. But they can inform, and help with decision-making. They can also be reassuring. Our belief is that you need to be informed to make decisions. And that might mean gathering information and then deciding not to make a decision. That’s a decision too! But our belief might not be your belief. Do what’s right for you.
The key to this is knowing what your options are. And if you need to make doubly sure that the options you have on the table are the right ones for you then think about a second opinion. The brain tumour pathway is increasingly very complex with combinations of treatments and with the better knowledge that we now have about the molecular make up of brain tumours, what is right for one person will not be right for the next. You should also know that you may hear that there are no other options and this can be distressing. What is key is that you are in charge and that the path that you choose is the right one for you. Do not worry about upsetting your clinicians – a good clinician will understand the need to seek other opinions in a diagnosis as serious as this.
There is lots to consider when thinking about seeking a second opinion. Read our Know How on how to get a second opinion here.
If you want to seek further opinions, you will need a copy set of scans. Ask your hospital for these. There are two ways of seeking a second opinion:
Visit your GP and ask for a second, even third opinions. If you want more information about where you might go and who might be appropriate to see, ask us at brainstrust, ask your consultant or your GP. Get your GP on your side – they can unlock so much for you.
We can also help. Contact hello@brainstrust.org.uk. We can’t give you a second opinion, but we know someone who can – at one of the leading neurosurgical centres in the UK.
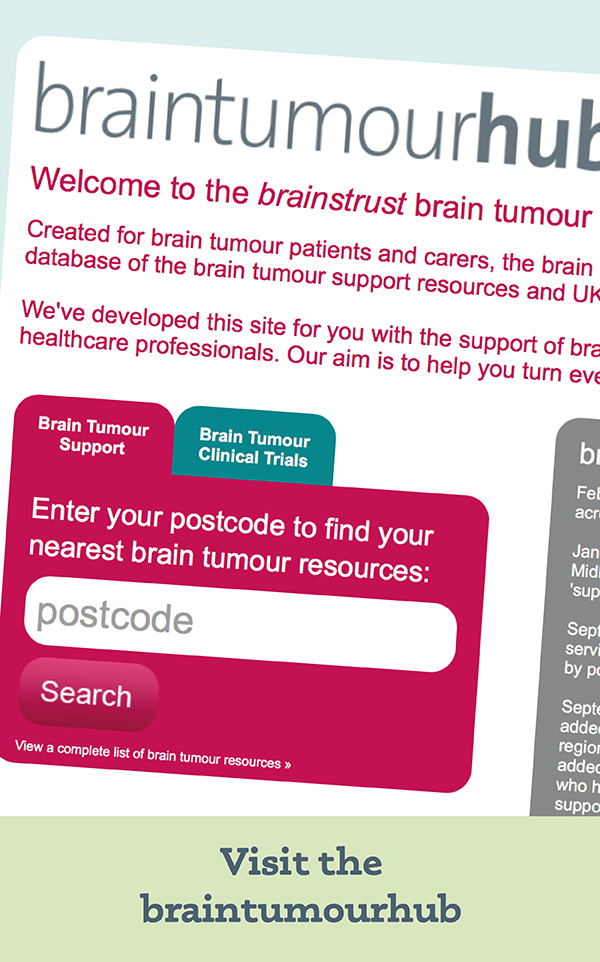
And then there is also Trustedoctor. Trustedoctor enables patients to access the right specialist anywhere in the world, regardless of geographical location. The comprehensive doctor profiles provide all of the information that a patient requires to decide for themselves who is the best fit for their specific condition. This resource enables you to:
- Search a global database for the best doctor for your needs.
- Upload your documents and a summary of your case.
- Receive a private, real-time video consultation within the Trustedoctor platform. Each consultation is followed up with a comprehensive written report.
- Share and discuss documents, scans and more during your consultation with your doctor using our live document viewer.
Trustedoctor specialists are hand-picked by a board of medical experts, based on a number of key factors:
- Clinical experience
- Academic impact
- Endorsement by peers and patients
- Their clinical network.
Finally, you will be frustrated but don’t expect answers from your healthcare team, unless you ask the question. That’s why it is so important to be informed. Once you accept this you will be able to handle the whole situation much more effectively. It took us a year to get to this point. Seek second, third, even fourth opinions and then try to stand back and draw out the key notes. Your position is not easy – you will be feeling like you are damned if you do and you’re damned if you don’t but at least you will be able to say that any decisions you have made have been informed decisions
Yesterday was the first time, for about a year, that we have been able to talk through my husband’s illness with someone in the medical profession who has been able to answer our questions with a full understanding of his illness.
Thank you so much for recommending that we go and see him.
Julie, carer, Sussex
brainstrust is here to help you get the most out of your team. Find out more about working with your team here.